Get the free Pharmacy Drug/product Prior Authorization Form
Get, Create, Make and Sign pharmacy drugproduct prior authorization



Editing pharmacy drugproduct prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out pharmacy drugproduct prior authorization

How to fill out pharmacy drugproduct prior authorization
Who needs pharmacy drugproduct prior authorization?
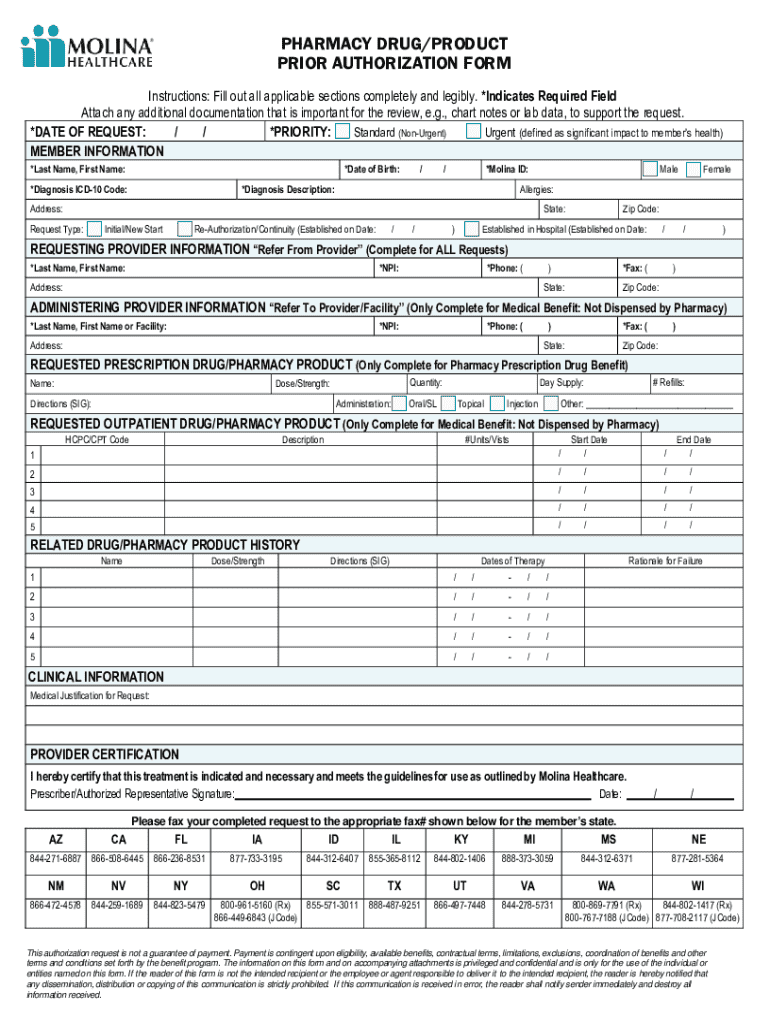
A comprehensive guide to pharmacy drug product prior authorization forms
Understanding prior authorization
Prior authorization (PA) in pharmacy is a process mandated by insurers to determine if a prescribed medication is medically necessary before coverage is approved. This requires healthcare providers to submit a request outlining the justification for the prescribed drug, supporting its clinical necessity over more cost-effective alternatives. Prior authorization serves a crucial function in healthcare, ensuring that treatments are appropriately aligned with medical guidelines and cost management strategies.
The importance of prior authorization forms cannot be overstated. They serve as vital communication tools between providers, pharmacists, and insurance companies. These forms contain essential details that substantiate the need for specific medications, streamlining approval processes while safeguarding against unnecessary spending. Understanding the nuances of the drug product prior authorization process is essential for both healthcare providers and patients, enhancing treatment access while ensuring compliance with health insurance policies.
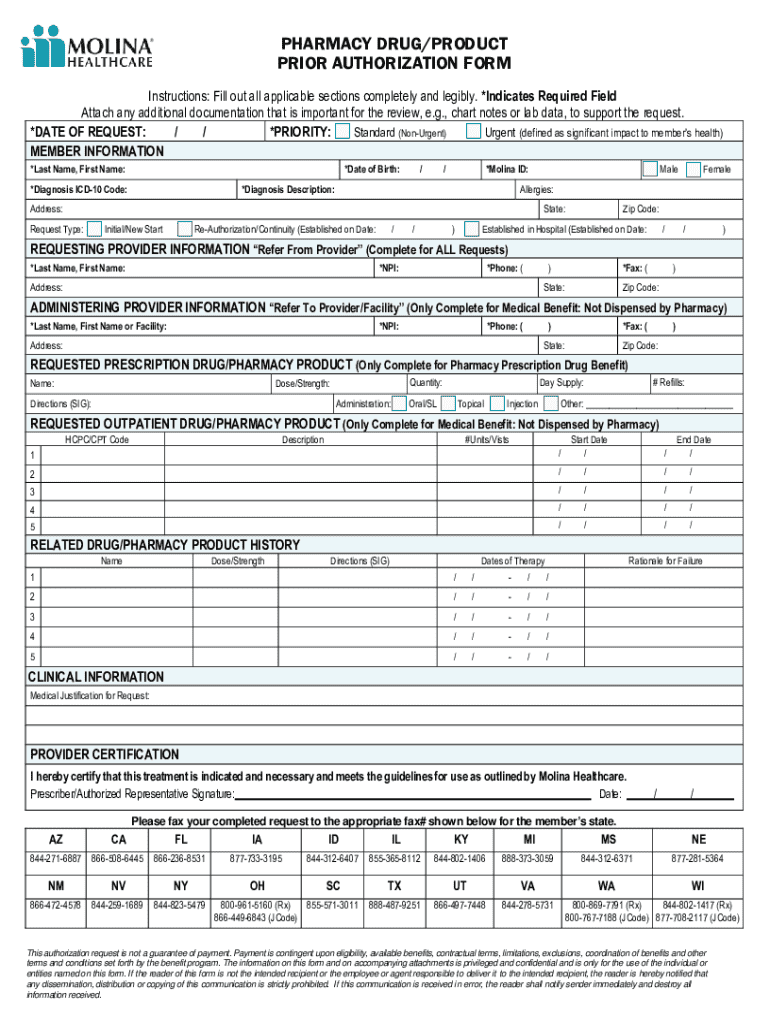
Key elements of a pharmacy drug product prior authorization form
Filling out a pharmacy drug product prior authorization form correctly requires preparation and attention to detail. Important components include patient information, which typically encompasses the patient's full name, date of birth, and insurance details to ensure correct identification and eligibility verification. Provider details, such as the prescribing physician's name, contact information, and National Provider Identifier (NPI), must also be included to establish authority and accountability.
Medication information is another critical element, which should clearly state the prescribed medication's name, dosage, route of administration, and the expected duration of therapy. In addition, attachments and supporting documentation are vital for a successful prior authorization submission.
Step-by-step guide to filling out the pharmacy drug product prior authorization form
Completing the prior authorization form is a systematic process that demands thoroughness and accuracy. Start by gathering the patient's data, ensuring it is up-to-date and compliant with HIPAA regulations. This means confirming that you have the correct name, date of birth, and insurer details before proceeding.
Creating a robust provider section is the next step. Include comprehensive details about the healthcare provider, such as their name, address, phone number, and NPI number. It's crucial to double-check these details, as errors can lead to significant delays in processing the request.
Specify the medication information clearly: mention the medication name, correct drug code, and dosage instructions alongside the anticipated duration of treatment. To further strengthen your case, include thorough supporting documentation. This might include clinical notes, test results, and history of treatments with alternative medications that were ineffective.
Before submitting the prior authorization form, review and verify all entries. Develop a checklist for completion, confirming each section is accurately filled out. Implementing a review stage is critical to avoiding common pitfalls that could lead to denial.
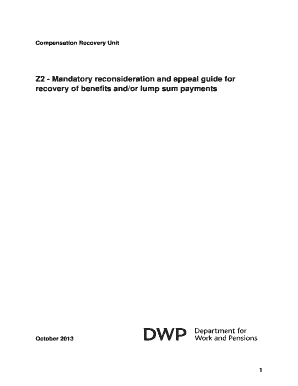
Common reasons for prior authorization denials
Prior authorization requests can be denied for several reasons, with incomplete or incorrect forms topping the list. Misunderstanding the medical necessity justifications required by insurers can lead to further complications, impacting patient access to needed medications. Additionally, non-adherence to specific policy guidelines set forth by the insurance provider often results in denials.
To improve approval chances, implement effective strategies such as ensuring that all documentation is thorough and aligns with the insurer’s requirements. Engaging in open communication with insurance company representatives can also provide clarity on evolving guidelines and expectations for medical necessity.
Resources for effective management of prior authorization forms
Utilizing interactive tools greatly enhances the efficiency of filling out pharmacy drug product prior authorization forms. Leveraging online templates and integrated editing features can streamline the completion process, particularly when multiple forms need to be filled out for various patients. eSigning capabilities simplify the submission process, reducing the downtime between submission and approval considerably.
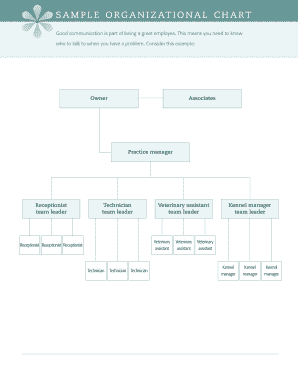
Moreover, collaboration features for healthcare teams can significantly improve workflow. Sharing forms with other team members allows for collective oversight and ensures that the most current information is reflected in the submissions. Tracking submission statuses and updates provides additional peace of mind, enhancing overall process effectiveness.
Best practices for healthcare providers managing prior authorizations
Developing an organized workflow is essential for managing prior authorizations efficiently. Tools and software designed specifically for this purpose can automate reminders for submissions, enabling timely responses to urgent requests. Prioritizing time management can relieve the burden frequently associated with processing these requests, making it easier for healthcare providers to focus on patient care.
Building strong communication channels with pharmacies and insurers facilitates quicker clarifications and information sharing. Ensure that you have contact points designated for inquiries and maintain awareness of policy changes that may occur. This proactive approach will prepare your team to navigate insurance issues and reduce the likelihood of delays.
Case studies - successful prior authorization submissions
Successful prior authorization submissions often hinge on the quality of documentation submitted. Case studies reveal that cohesive documentation where all elements are clearly articulated can make significant differences in obtaining approval. For instance, a case involving a patient with a chronic condition was supported by detailed clinical notes and a thorough treatment history, leading to swift approval from the insurance provider.
Analyzing approved requests and the feedback received from insurers provides useful insights that can inform future submissions. These case studies underscore the value of constructing a comprehensive narrative that outlines clinical necessity and supports the case for the prescribed medication.
Maximizing the benefits of using pdfFiller for prior authorization
pdfFiller is designed to facilitate efficient document handling, particularly in managing pharmacy drug product prior authorization forms. Its features can significantly save time and effort, from seamlessly editing PDFs to providing e-signature functionalities that provide instant acknowledgment and processing.
The platform offers tailored solutions suitable for both individual users and teams, ensuring that all members benefit from cloud-based document access at any time. This enhances collaboration and fosters an environment of efficiency, addressing the specific needs of healthcare providers aiming for impactful patient outcomes.
Navigating challenges in prior authorization submissions
Healthcare providers often face challenges when submitting prior authorization requests, especially when dealing with urgent requests that require expedience. It's critical to have a streamlined process in place to triage these requests, ensuring that necessary information is prioritized. Developing a checklist or a procedural guide can assist in maintaining a level of urgency without sacrificing quality.
For cases where prior authorizations are denied, knowing the appeals process is paramount. Understanding the specific reasons for denial can equip providers to craft a compelling resubmission or appeal argument that addresses those concerns directly. Moreover, creating a collaborative environment within the healthcare team can empower staff to share and strategize collectively, boosting the success rates of appeals.
Future trends in pharmacy drug product prior authorizations
As healthcare continues to evolve, so does the landscape of prior authorization processes. Technological innovations are on the rise, including artificial intelligence and machine learning tools that aim to simplify and expedite the prior authorization process. These technologies can reduce administrative burden, allowing healthcare professionals to focus more on patient care rather than paperwork.
Moreover, the policy landscape surrounding prior authorizations is also changing. Stakeholders are increasingly promoting patient-centered approaches aimed at minimizing barriers to access, particularly for critical medications. Understanding these trends is essential for healthcare providers to effectively navigate upcoming changes and advocate for their patients.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find pharmacy drugproduct prior authorization?
How do I complete pharmacy drugproduct prior authorization on an iOS device?
How do I edit pharmacy drugproduct prior authorization on an Android device?
What is pharmacy drug product prior authorization?
Who is required to file pharmacy drug product prior authorization?
How to fill out pharmacy drug product prior authorization?
What is the purpose of pharmacy drug product prior authorization?
What information must be reported on pharmacy drug product prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.