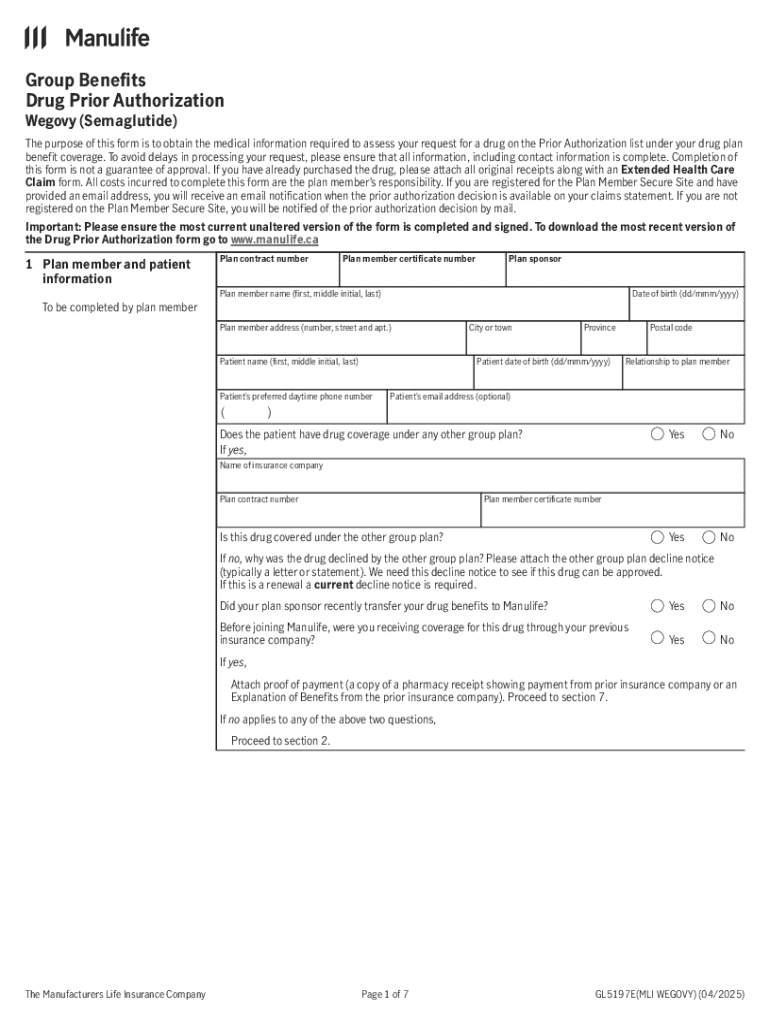
Get the free Drug Prior Authorization Form for Wegovy
Get, Create, Make and Sign drug prior authorization form



How to edit drug prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out drug prior authorization form

How to fill out drug prior authorization form
Who needs drug prior authorization form?
Understanding Drug Prior Authorization Forms: A Comprehensive Guide
Understanding drug prior authorization
Drug prior authorization is a process required by insurance companies to determine if they will cover medication prescribed by a healthcare provider. Before patients can access certain drugs, their insurers require a formal request to justify their medical necessity. This precaution aims to ensure patient safety, encourage appropriate medication use, and control healthcare costs. Understanding this process is essential for patients, healthcare providers, and administrators.
Prior authorization plays a critical role in healthcare management. It serves to filter out potentially unnecessary treatments, ultimately aiming to lower overall healthcare costs while ensuring patients receive effective medications. Common medications that often require prior authorization include specialty drugs such as biologics, antidepressants, and high-cost oncology treatments.
Navigating the drug prior authorization process
Navigating the drug prior authorization process requires knowledge of how to initiate and complete requests effectively. Understanding the distinct phases of this process can reduce wait times and improve patient outcomes. The following outlines the key steps involved in obtaining prior authorization:
Completing the drug prior authorization form
Completing the drug prior authorization form accurately is key to obtaining timely approval. Each section must be filled with care to avoid delays. Here’s a detailed breakdown of the form's sections:
To avoid common mistakes, keep clarity and detail in mind when filling out each section. Omissions or vague answers can lead to unnecessary delays or denials.
Submitting the form
Once the form is completed, the next step is submission. There are various methods to submit the drug prior authorization form, including online submission via insurance portals, faxing the completed document, or mailing it directly to the insurance provider. After submission, it's crucial to understand what to expect. Approval timeframes can vary, but generally, responses are received within a few days to two weeks.
Communication from insurance providers may include approval notifications, requests for additional information, or denial letters. Staying proactive during this phase can enhance your chances of a successful outcome.
Follow-up actions
Understanding the approval or denial process is vital for effective management of the drug prior authorization. If a request is denied, there are specific steps that can be taken. First, familiarize yourself with the reason for denial. This information will guide you in formulating a response and may include appealing the decision by clarifying the clinical necessity of the medication.
Successfully navigating the appeal process can significantly impact patient care, ensuring timely access to necessary medications.
Managing future prescriptions with prior authorization
For ongoing management, establishing a systematic approach can streamline the drug prior authorization process. Key practices include maintaining organized documentation and becoming familiar with the rules for re-authorization for new prescriptions. Staying informed about updates from insurance providers is pivotal.
Utilizing tools such as pdfFiller can enhance your document management experience, providing an efficient platform to fill, edit, and sign forms seamlessly.
Building a comprehensive prior authorization strategy
Integrating prior authorization within your healthcare workflow is essential for effective operation, particularly in environments with high prescription volumes. Utilizing interactive tools can improve management efficiency and reduce the administrative burdens placed on healthcare teams.
Resources and tools for drug prior authorization
Accessing the right resources can significantly ease the complexities of the drug prior authorization process. pdfFiller offers numerous tools specifically designed to assist in creating and managing drug prior authorization forms. Links to common prior authorization forms can be beneficial, as well as gaining access to interactive tools through pdfFiller that streamline the submission process for patients and providers alike.
Leveraging pdfFiller for your document needs
pdfFiller’s cloud-based document solutions empower users by simplifying the editing, signing, and collaborating aspects of document management. This platform not only facilitates seamless interaction with forms like the drug prior authorization form but also enhances user efficiency with its easy-to-navigate features.
The benefits of adopting pdfFiller for managing prior authorization requests include enhancing turnaround times for form submissions, ensuring compliance with regulations, and improving team collaboration. User testimonials highlight the effectiveness of pdfFiller in resolving common pain points related to prior authorization management.
Contact information for support
If you need additional help with the drug prior authorization process or navigating pdfFiller, customer support is readily available. pdfFiller provides resources, FAQs, and direct support channels to assist users throughout their document management journey efficiently.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send drug prior authorization form for eSignature?
How do I make changes in drug prior authorization form?
How do I edit drug prior authorization form in Chrome?
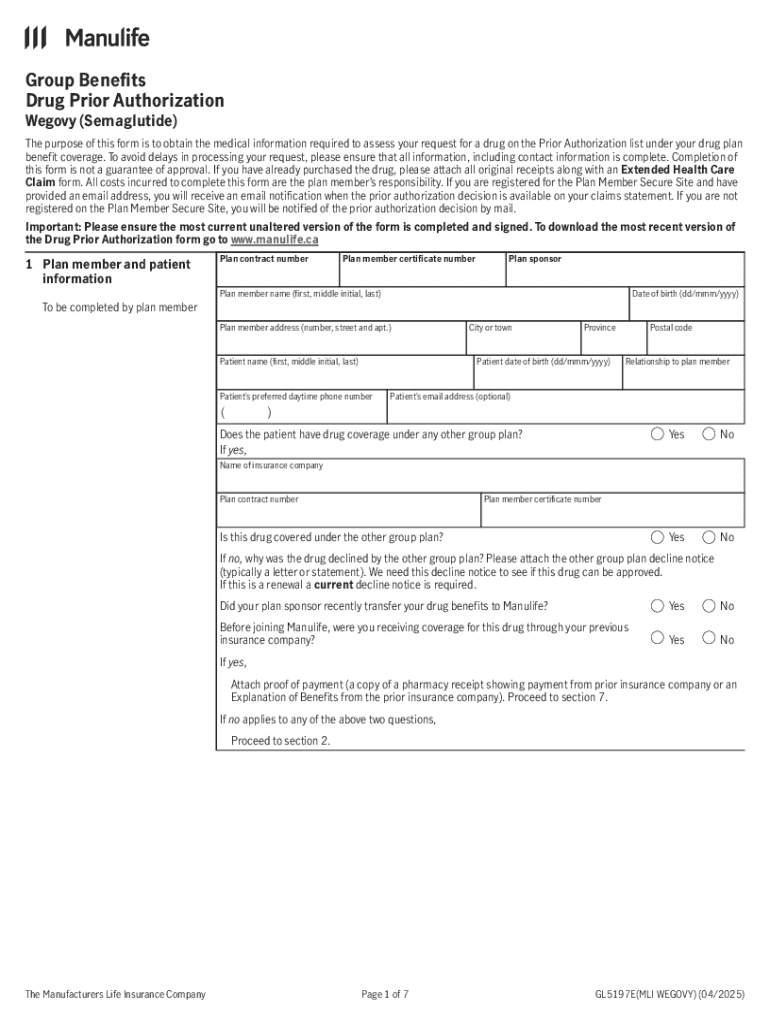
What is drug prior authorization form?
Who is required to file drug prior authorization form?
How to fill out drug prior authorization form?
What is the purpose of drug prior authorization form?
What information must be reported on drug prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.