Get the free Androgenic Agents (topical ) Prior Authorization (pa)
Get, Create, Make and Sign androgenic agents topical prior



Editing androgenic agents topical prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out androgenic agents topical prior

How to fill out androgenic agents topical prior
Who needs androgenic agents topical prior?
Androgenic agents topical prior form: A comprehensive guide
Understanding androgenic agents: A comprehensive overview
Androgenic agents, primarily associated with the male hormone testosterone, are compounds that can promote male characteristics such as increased muscle mass and bone density. In topical forms, these agents are applied directly to the skin, allowing for localized effects while minimizing systemic absorption. Topical androgenic agents are essential for treating various conditions, including androgen deficiency, hair loss, and certain dermatological disorders.
The importance of topical application lies in its ability to deliver therapeutic agents directly to the affected area, resulting in improved efficacy and reduced side effects. For instance, patients dealing with androgen-related hair loss can benefit significantly from topical treatments, as they concentrate the androgenic effects right where they are needed. Common conditions treated with these agents include alopecia, hypogonadism, and some skin conditions that respond favorably to androgens.
The role of prior authorization in androgenic treatments
Prior authorization is a crucial step in the healthcare process where insurance companies review the medical necessity of a requested treatment before approving coverage. This step ensures that patients receive appropriate and necessary care while also managing healthcare costs. For androgenic agents, prior authorization is especially vital due to the potential for misuse and the need for careful patient monitoring.
The approval process involves several key stakeholders, including the prescribing physician, the insurance provider, and the patient. Physicians must provide detailed documentation supporting the need for the specified treatment, while insurance companies assess this information to ensure compliance with their guidelines.
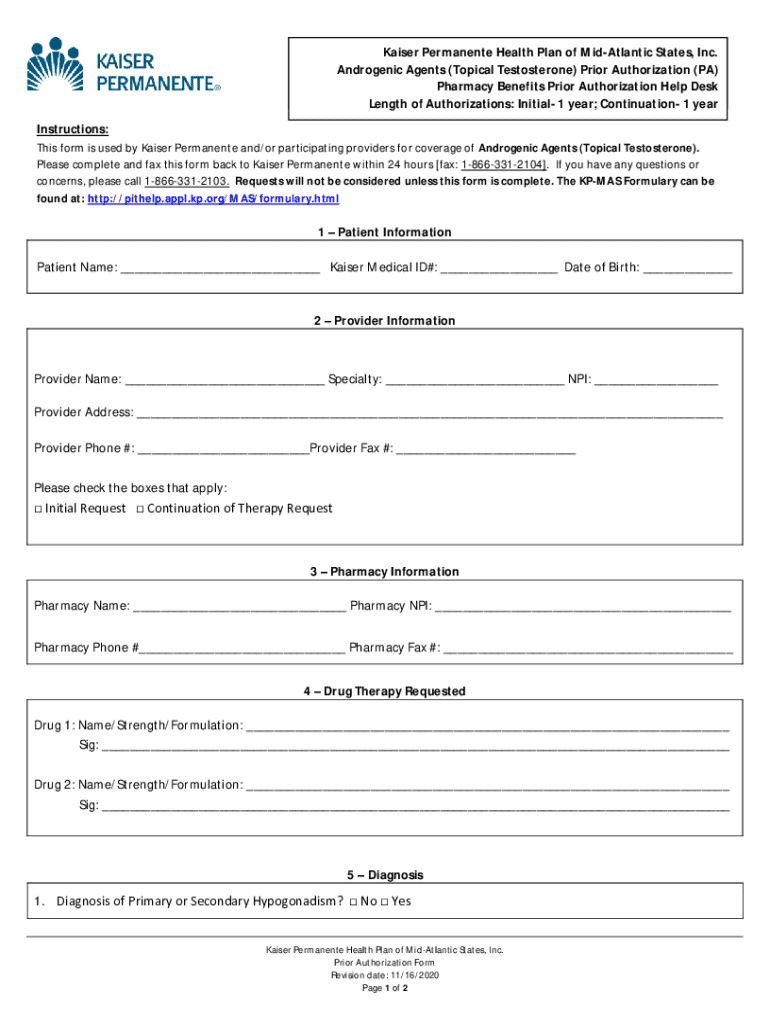
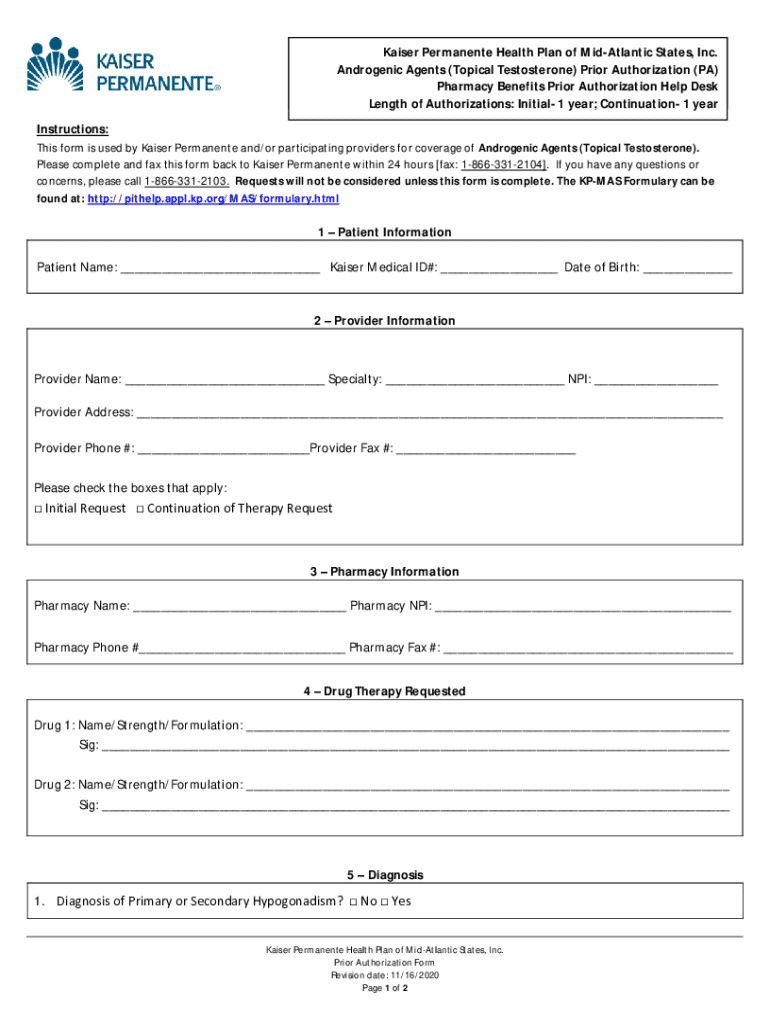
Navigating the topical prior form for androgenic agents
Completing the topical prior form for androgenic agents is a structured process aimed at ensuring all necessary information is captured accurately. This form typically requires detailed patient and prescriber information and specifics regarding the medication. By understanding the required elements, you can expedite the approval process.
The required information generally includes:
Filling out the form involves several steps: 1) Gather necessary documentation that supports the medical need, 2) Complete the patient’s medical history, 3) Document treatment justification, and 4) Ensure accurate medication information. Each of these steps is integral to presenting a compelling case for the prior authorization request.
Submission process for the prior form
Submitting the prior form can be done through various methods, providing flexibility based on the prescriber's preferences. Common submission methods include online portals, fax submissions, and traditional mail. It's essential to choose the method that aligns best with the patient's and provider's capabilities.
The timeline for approval can vary, often ranging from a few days to several weeks. It's important to be aware of common roadblocks such as incomplete submissions or documentation requirements. Understanding these timelines can help manage patient expectations regarding treatment initiation.
Understanding the approval criteria for androgenic agents
Insurance companies employ specific criteria to determine the approval of androgenic agents. The primary considerations include medical necessity, prior treatment trials, and thorough documentation. Medical necessity often requires clinical evidence that justifies the need for topical androgenic treatment. Additionally, insurance providers frequently mandate that patients undergo previous treatments before considering androgenic agents.
Documentation requirements typically involve detailed medical histories, treatment records, and justification of the need for the specific medication. Typical approval timelines can vary, with follow-up steps often needed to clarify any outstanding questions from the insurer.
Common errors to avoid in the submission process
Errors in the submission process for prior authorization can lead to unnecessary delays or denials. One common mistake is providing incomplete information, which may prevent the insurance provider from making an informed decision. Additionally, insufficient supporting documentation can also impact the approval outcome.
Here's a list of common errors to avoid:
What to do if your prior authorization is denied
Receiving a denial for prior authorization can be disheartening, but it's not the end of the road. The first step after a denial should be to carefully review the reasons provided by the insurance company. Most denials occur due to inadequate justification or failure to meet criteria. Understanding these reasons can guide you in addressing the objections raised.
To appeal a denied authorization, follow these key steps:
Utilizing available resources such as patient advocacy groups or professional associations can provide additional support in navigating the appeal process.
Interactive tools for managing your androgenic treatment forms
Utilizing tools like pdfFiller can significantly streamline the document creation process, particularly when dealing with prior authorization forms for androgenic agents. This platform offers innovative features that enhance the user experience, making it more manageable to complete necessary documentation and ensure accuracy.
Key features include:
Frequently asked questions about topical androgenic agents and prior forms
Clarifications on common misconceptions about topical androgenic agents can help patients and providers navigate the complexities of treatment effectively. Patients often have rights regarding their treatment choices and responsibilities to inform providers about their medical history.
In this section, we'll address:
Contact and support information
For immediate assistance with your androgenic agents topical prior form, you can reach out to dedicated helplines provided by your health insurance company or local healthcare providers. These resources can help clarify questions about the prior authorization process and provide guidance on next steps.
Additionally, pdfFiller offers a range of resources for providers and patients, ensuring you have access to tools and services to aid in document management. Their hours of operation typically include standard business hours, providing ample opportunity for support.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for the androgenic agents topical prior in Chrome?
How do I edit androgenic agents topical prior on an iOS device?
How do I complete androgenic agents topical prior on an iOS device?
What is androgenic agents topical prior?
Who is required to file androgenic agents topical prior?
How to fill out androgenic agents topical prior?
What is the purpose of androgenic agents topical prior?
What information must be reported on androgenic agents topical prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.