Get the free Prior Authorization Request
Get, Create, Make and Sign prior authorization request
How to edit prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request
How to fill out prior authorization request
Who needs prior authorization request?
Prior Authorization Request Form - How-to Guide Long-Read
Understanding the prior authorization request form
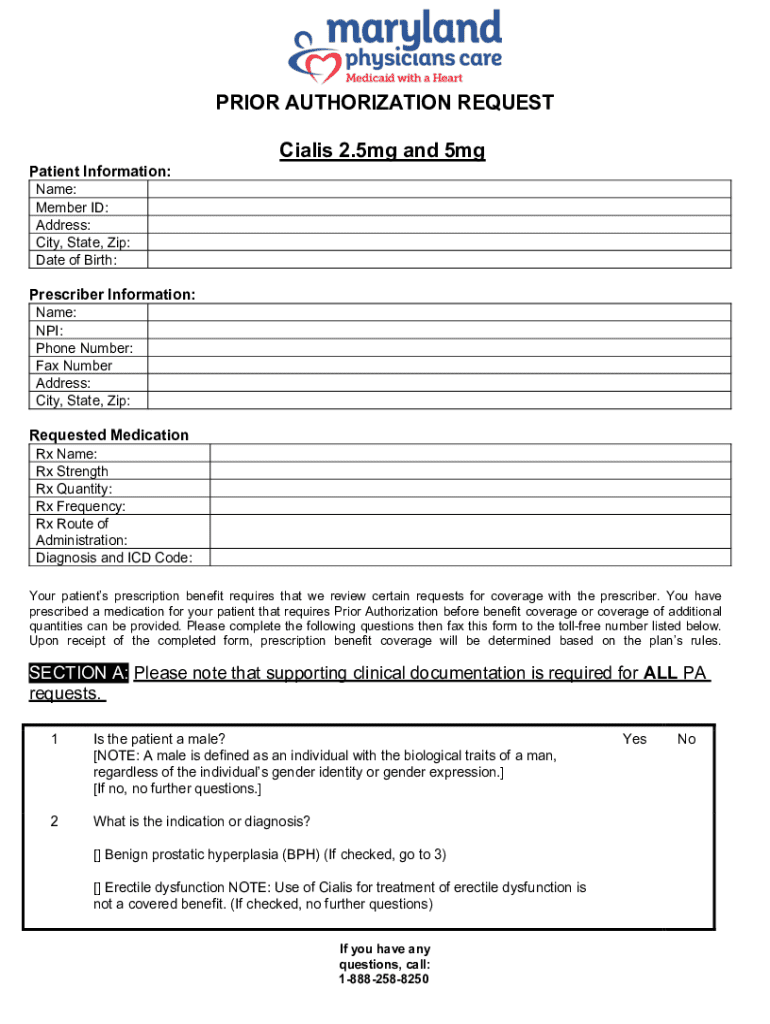
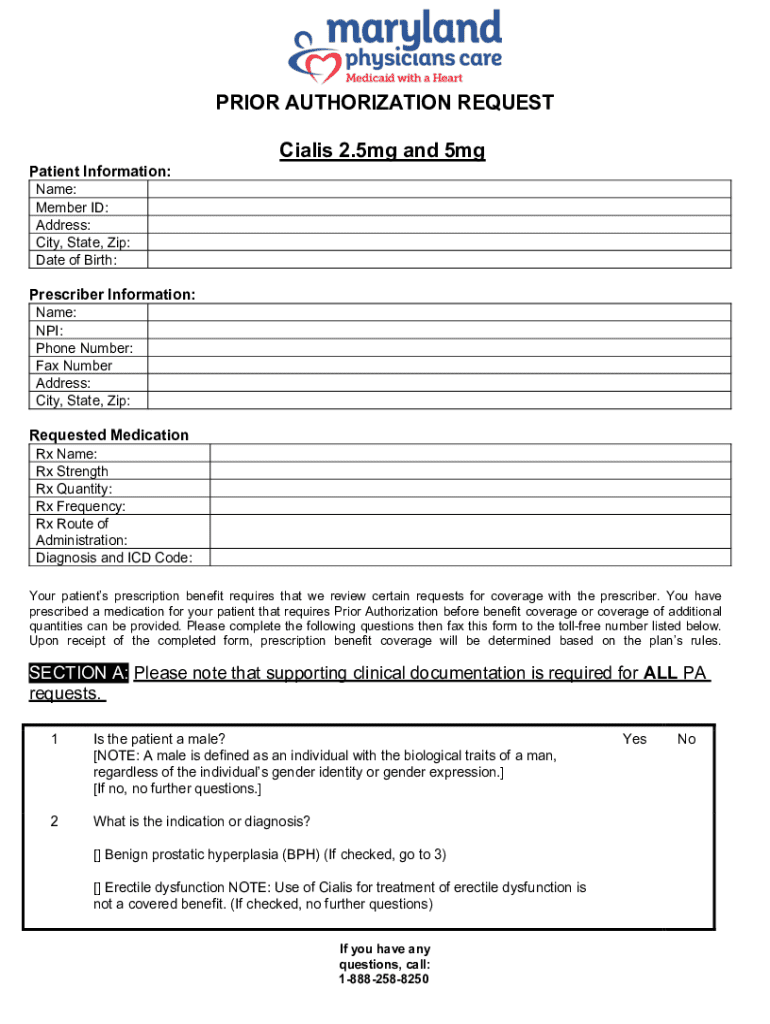
A prior authorization request form is a crucial document in healthcare that healthcare providers must complete to obtain approval from insurance companies before a specific service, medication, or treatment is administered to a patient. This form not only serves as a formal request but also as a means to justify the need for specific healthcare services based on medical necessity. Without prior authorization, patients may face unexpected denials from insurance providers, leading to significant out-of-pocket expenses.
The importance of the prior authorization process cannot be understated. It helps control healthcare costs and ensures that patients receive appropriate and necessary care while minimizing the number of unnecessary treatments. Furthermore, it serves as a checkpoint for providers and patients to review patient care strategies together, promoting better health outcomes.
Common uses for a prior authorization request form include requests for high-cost medications, specialized diagnostic tests, elective surgeries, and referrals to specialists. In many cases, health insurance plans will require this form to ensure that the procedures or prescriptions being requested align with established medical guidelines and cost-effectiveness.
Key components of the prior authorization request form
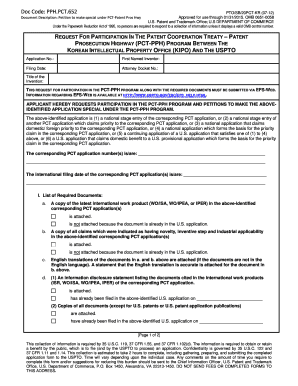
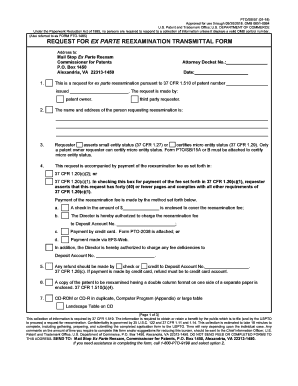
Understanding the key components of the prior authorization request form is essential for healthcare providers. Each submission requires specific information to ensure that it is processed swiftly and accurately. The essential information required encompasses three main areas: patient details, provider information, and details about the service or medication being requested.
In addition to the basic information, supporting documentation is often required. This may include medical records, lab results, or clinical notes that support the necessity for the requested service. Gathering and organizing these documents can streamline the approval process. It's important to double-check the requirements from the specific insurer, as they can vary.
Step-by-step guide to completing the prior authorization request form
Completing a prior authorization request form can seem daunting, but by following a step-by-step approach, healthcare providers can ensure accuracy and efficiency. Start by gathering necessary information, which includes a checklist of required details that you should have ready before filling out the form:
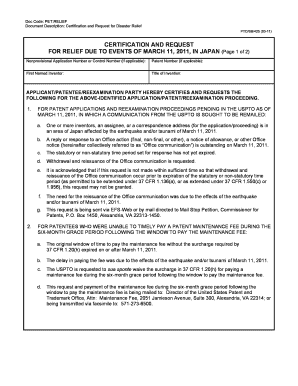
Once you have all the necessary information, you can move on to filling out the form. Carefully follow the structured sections, ensuring you input details accurately. Be mindful of any specific notes provided by the insurance company regarding the format or additional requirements.
After completing the form, it’s critical to review and edit it before submission. This step includes verifying the correctness of the entered information, checking for any missing elements, and ensuring that all required documentation is attached. Common mistakes to avoid include leaving fields blank, entering incorrect medical codes, and submitting without verifying insurance requirements.
Digital options for submitting the prior authorization request
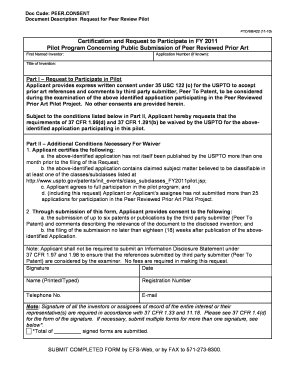
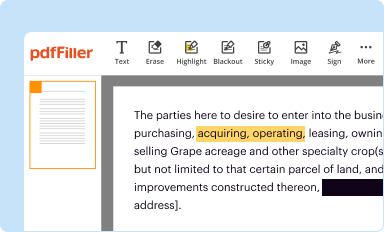
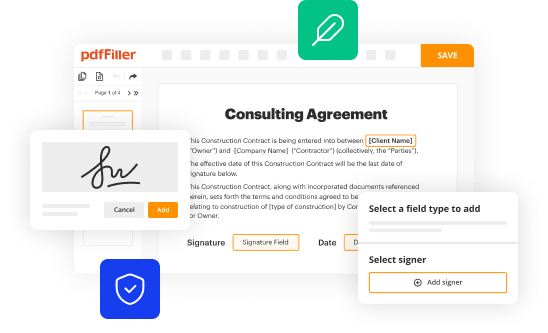
With the evolution of technology, online submission tools have become a preferred method for submitting prior authorization requests. These digital forms present numerous advantages, including the ability to access them from anywhere and streamline the review process. One such tool is pdfFiller, which enables users to create, edit, and submit prior authorization request forms with ease.
Using pdfFiller to facilitate the submission process can significantly reduce time and effort required for managing forms. The platform allows healthcare providers to fill out forms digitally, thus minimizing the risks associated with lost paperwork or error-filled submissions. Additionally, integrating electronic signature capabilities means that once the form is completed, it can be reviewed and signed without physically printing or faxing.
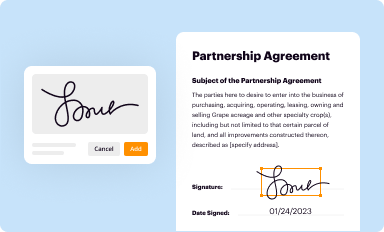
Electronic signature integration
The benefits of incorporating eSigning into the prior authorization request process cannot be overstated. eSigning not only speeds up the approval timeline but also ensures that documents are securely transmitted. To eSign a completed form in pdfFiller, users simply navigate to the relevant form, select the eSign option, and follow the prompts to complete the electronic signature process.
Tracking your prior authorization request
Following up on a prior authorization request is a vital step in the process that can greatly impact patient care. After submitting the request, it is important to check its status regularly to stay informed about any updates or additional information requests from the insurer.
Understanding the types of responses is equally important. You can typically expect either an approval or denial. If approved, you can proceed with the treatment. In the event of a denial, it’s crucial to understand the reasoning behind it and determine next steps
FAQ: Common questions about the prior authorization request form
There are frequently asked questions regarding the prior authorization request form, particularly about procedures following a denial, timelines, and appeal processes:
Case studies: Real-life examples of filling out prior authorization requests
Learning from real-life experiences can provide valuable insights into the prior authorization process. For instance, a successful authorization case could involve a patient who needed a costly MRI. The provider thoroughly filled out the prior authorization request form with supporting documentation, leading to rapid approval and facilitating timely diagnostic care.
Conversely, handling denials can provide lessons in diligence. A healthcare provider may have submitted a request without adequate documentation, leading to a denial. Understanding the grounds for denial allowed the provider to gather the necessary documentation and successfully appeal the decision, highlighting the importance of careful preparation.
Best practices shared by seasoned healthcare professionals emphasize the importance of clear communication with insurance representatives and ensuring that all requests are fully documented with relevant clinical information.
Leveraging technology for easier document management
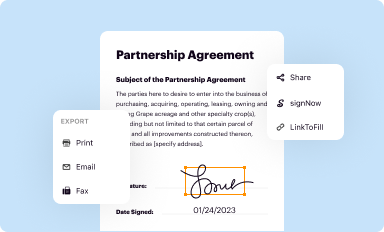
Utilizing technology can significantly enhance the effectiveness of managing prior authorization requests. pdfFiller is an excellent resource for editing and managing your forms, making it a versatile tool for healthcare providers. Its seamless editing capabilities allow users to fill in forms, sign them electronically, and store them securely.
Moreover, pdfFiller offers collaborative features that enable teams to work together on prior authorization requests, reducing the chances of error and ensuring comprehensive documentation. Other relevant tools also facilitate document storage and sharing, and custom templates tailored to specific needs can be created, streamlining workflows.
Enhancing your workflow with prior authorization management
Integrating prior authorization requests into daily healthcare operations can significantly improve workflow efficiency. This involves training your team on effective use of the prior authorization request form and ensuring everyone is aware of updated policies and procedures from insurance providers.
By keeping up with policy changes, providers can proactively adjust their processes, reducing delays and improving patient care. Regular training sessions can help maintain a well-informed team who can adeptly navigate the complexities of prior authorization.
Security measures when handling personal health information
When handling prior authorization request forms, security is paramount. Protecting personal health information (PHI) is not just a regulatory requirement but a critical aspect of maintaining patient trust. Ensuring that document management systems, such as pdfFiller, employ high-level encryption can safeguard sensitive data during transmission and storage.
Best practices for safeguarding documents include limiting access to authorized personnel, implementing secure passwords, and regularly updating systems to protect against vulnerabilities. pdfFiller takes security seriously, ensuring that user data is not only encrypted but also compliant with health privacy laws.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit prior authorization request from Google Drive?
How can I get prior authorization request?
Can I create an eSignature for the prior authorization request in Gmail?
What is prior authorization request?
Who is required to file prior authorization request?
How to fill out prior authorization request?
What is the purpose of prior authorization request?
What information must be reported on prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.