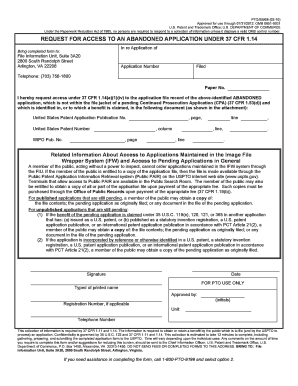
Get the free Drug Prior Authorization Form
Get, Create, Make and Sign drug prior authorization form



Editing drug prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
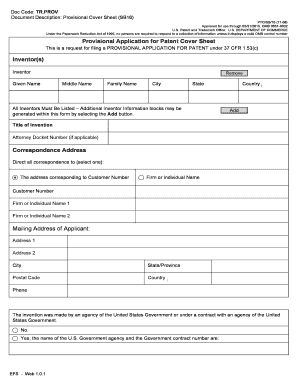
How to fill out drug prior authorization form

How to fill out drug prior authorization form
Who needs drug prior authorization form?
Drug Prior Authorization Form: How-to Guide Long-Read
Understanding drug prior authorization
Prior authorization is a critical step in the healthcare system, ensuring that patients receive necessary medications while managing costs for insurers. It acts as a gatekeeper for prescribed drugs that may be expensive or require special circumstances for dispensing.
The importance of prior authorization cannot be overstated. It serves to protect patients from the high costs of certain medications, while also requiring healthcare providers to justify the need for specific treatments. This process can significantly influence treatment decisions and access to medications.
Medications that commonly require prior authorization include those used for complex conditions, such as cancer treatments, biologics, or drugs with high potential for abuse. Understanding which prescriptions need authorization can expedite the process and reduce delays in patient care.
The prior authorization process typically involves submitting a request to the insurance provider, who will review it based on established criteria. This could include evaluating the patient's medical history, the prescribed drug's effectiveness, and other treatment alternatives.
The drug prior authorization form: An overview
The drug prior authorization form serves a pivotal role in this process. Its primary purpose is to collect and communicate essential information about the patient's medical condition and the prescribed medication to the insurer. This form ensures the review is comprehensive and accurate.
Key elements of the drug prior authorization form include:
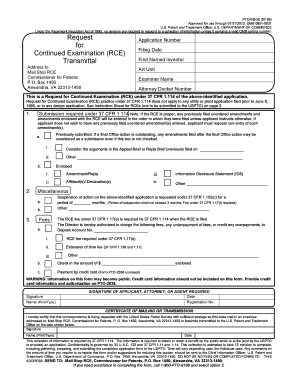
Step-by-step guide to filling out the drug prior authorization form
Filling out the drug prior authorization form can be complex, but by following a systematic approach, you can enhance accuracy and efficiency.
Gathering required information
Start by gathering the patient's medical history, which may include previous diagnoses, treatment history, and responses to prior medications. Additionally, obtain a comprehensive medication history that outlines all prescriptions, over-the-counter drugs, and supplements currently being taken.
Completing the form
Carefully complete each section of the form, ensuring that you provide precise and clear details. Common mistakes to avoid include omitting information, unclear handwriting, and failing to provide necessary supporting documents, which can lead to delays in approval.
Reviewing the completed form
Before submitting, conduct a thorough review of the completed form using a checklist to catch any errors or omissions. Key aspects to verify include patient details, prescriber details, and any additional notes or supporting documentation required by the insurer.
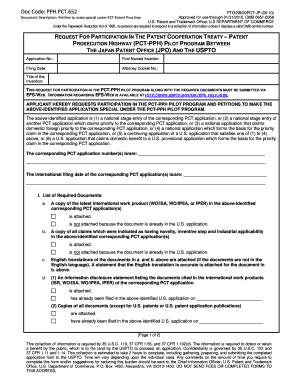
Submitting the drug prior authorization form
Once you have filled out the form, the next step is submission. There are several methods available for submitting the drug prior authorization form.
Methods of submission
What to expect after submission
After submission, you can expect a response within a specific timeframe, depending on the insurance provider's policies. Common follow-up actions may include contacting the insurer to check the status of the request, especially if you haven’t received a response.
Denial and appeal process
Not every prior authorization request is approved; understanding the reasons behind denials is crucial for improving future requests.
Understanding denials
Common reasons for denial may include incomplete forms, lack of medical necessity, or failure to follow the insurer's specific guidelines. Knowing these reasons can help healthcare providers better prepare future submissions.
Steps to appeal a denial
Tools and resources for managing drug prior authorization
Navigating the complexities of drug prior authorization requires the right tools and resources. Platforms like pdfFiller offer a variety of interactive tools that can streamline this process.
Interactive tools on pdfFiller
Additional resources
Best practices for handling drug prior authorization requests
Effective management of prior authorization requests can lead to improved patient outcomes and smoother processes for healthcare providers.
Conclusion
Understanding and successfully navigating the drug prior authorization form is fundamental for both healthcare providers and patients. Proactive management not only improves the chances of approval but also enhances the overall efficiency of care delivery.
By familiarizing yourself with the details and best practices outlined in this guide, you can streamline the prior authorization process, ensuring that both you and your patients can focus on what matters most: effective treatment and care.
Support and contact information
Should you need assistance with the drug prior authorization form, support is available. Contacting customer support can clear up any uncertainties and provide guidance on navigating common challenges.
Contacting customer support
Footer menu






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my drug prior authorization form in Gmail?
How do I edit drug prior authorization form in Chrome?
Can I sign the drug prior authorization form electronically in Chrome?
What is drug prior authorization form?
Who is required to file drug prior authorization form?
How to fill out drug prior authorization form?
What is the purpose of drug prior authorization form?
What information must be reported on drug prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.