Get the free Medical Prior Authorization
Get, Create, Make and Sign medical prior authorization



How to edit medical prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medical prior authorization

How to fill out medical prior authorization
Who needs medical prior authorization?
A Comprehensive Guide to Medical Prior Authorization Forms
Understanding medical prior authorization
Medical prior authorization serves as an essential process in healthcare, allowing insurance companies to review and approve specific medical services before they are administered. The primary purpose of this requirement is to ensure that the proposed treatment or procedure aligns with the patient’s medical needs and the insurance policy's guidelines. Consequently, it plays a critical role in controlling healthcare costs and enhancing patient safety.
The importance of medical prior authorization extends beyond mere cost management; it also acts as a safeguard for patients, ensuring that only medically necessary treatments are covered. By requiring prior approval, insurance companies can help prevent unnecessary procedures that may expose patients to risks without providing significant benefits.
Who requires prior authorization?
Prior authorization is commonly required for a variety of services and procedures. These typically include high-cost imaging services (like MRIs and CT scans), specialty medications, surgeries, and non-emergency hospital admissions. Understanding which services necessitate prior authorization is critical for both patients and providers to avoid unexpected denial of coverage and ensure the timely delivery of care.
Healthcare providers, particularly physicians and specialists, are responsible for obtaining these approvals. They must be familiar with their patients' insurance policies and the specific criteria for the required prior authorization to facilitate a smooth process.
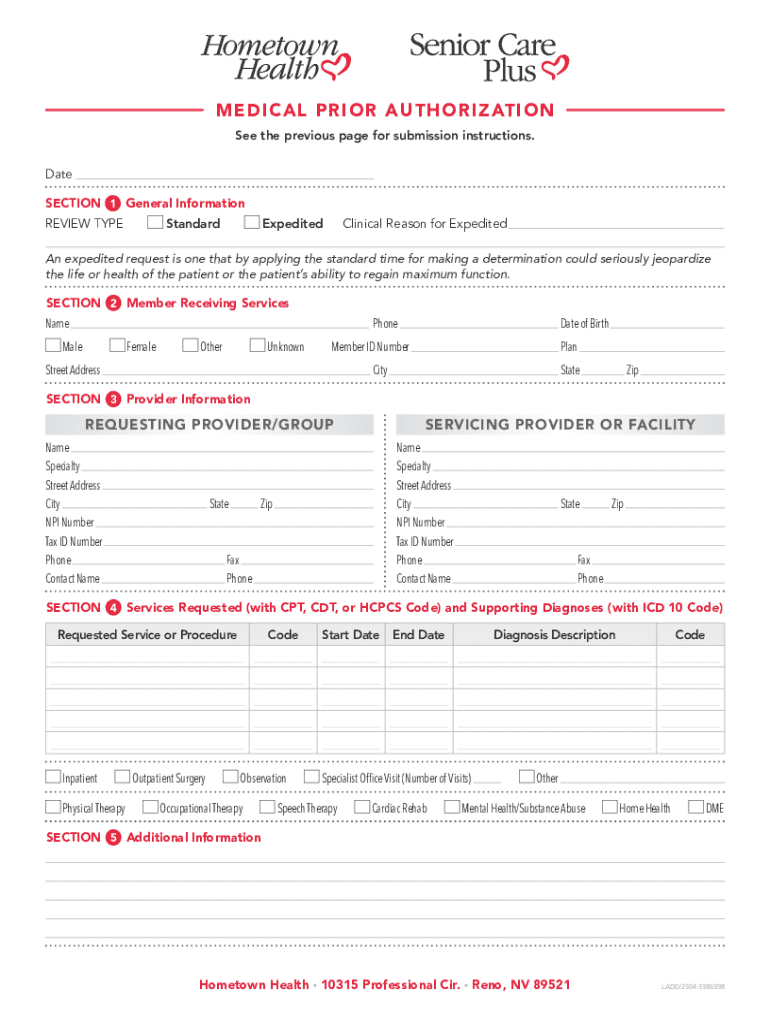
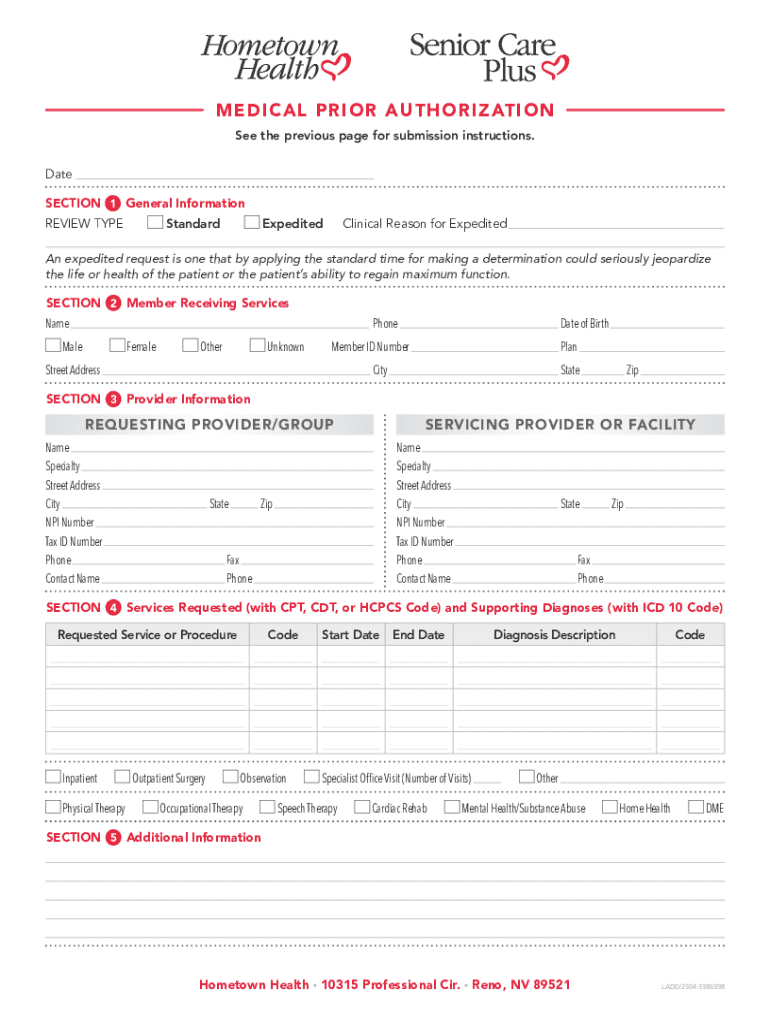
Key components of the medical prior authorization form
A medical prior authorization form needs to capture essential information to be considered complete and actionable. Key elements of this form include:
Despite the essential role of the authorization form, common mistakes can lead to unnecessary delays or denials. These include incomplete sections, incorrect coding, and discrepancies between requested services and provided justifications. Ensuring accuracy and thoroughness at the outset can mitigate these risks.
Step-by-step guide to filling out the form
Filling out a medical prior authorization form may initially seem daunting, but breaking it down into manageable steps can streamline the process.
Step 1: Gather necessary documentation
Before tackling the form, prepare by gathering the following documentation:
Step 2: Complete patient information section
Ensure that all fields are accurately filled with up-to-date information. This includes the patient's full name, date of birth, insurance plan type, and policy number. These details are the foundation for the remainder of the process.
Step 3: Detail the requested service
Clearly describe the medical service being requested. Include precise information such as procedure codes and descriptions to minimize the risk of misinterpretation by the insurance provider.
Step 4: Provide supporting medical necessity
Medical necessity is a critical component of the prior authorization process. This concept highlights that the requested service is not only needed but is also appropriate in terms of the patient’s health condition. Supporting documentation might include:
Step 5: Review and verify information
Once the form is filled, conduct a thorough review to ensure all information is complete and accurate. Double-check that all necessary documentation is attached, then use a checklist to confirm that no critical information has been omitted.
Editing and finalizing the medical prior authorization form
The editing process can be streamlined using tools like pdfFiller. This platform provides a user-friendly interface for making adjustments to the medical prior authorization form, ensuring it meets all submission standards.
To access and utilize pdfFiller’s editing features, follow these steps:
Digital signatures are often a necessity for the completion of forms like these. pdfFiller allows users to sign documents electronically, which not only saves time but also enhances the security of the process. If collaboration with team members is required, the platform’s sharing options simplify this process, allowing for smooth communication and feedback collection.
Submitting the form
Once the medical prior authorization form is complete and finalized, the next critical step is submission. There are several methods for submission, each with its benefits.
Different submission methods available
1. **Electronic submissions**: Many insurance companies now prefer electronic submissions, which can be completed directly through their online portals. This method often speeds up the response time and enables easy tracking.
2. **Paper submissions**: If electronic submission is not feasible, printed versions can be mailed. It's advisable to use certified mail to have proof of delivery.
Understanding submission timelines
Submission timelines can vary significantly depending on the insurance provider and the complexity of the request. Generally, providers can expect a response within a few business days but should check specific policies with the insurer.
Tracking your submission
Utilizing tools within the pdfFiller platform, or checking with the insurance company’s portal, can help you monitor the status of your prior authorization request. Keeping organized records and tracking communication can significantly minimize confusion and delays.
Managing and updating your prior authorizations
Once a prior authorization is granted, it's crucial to maintain an organized system for managing these requests. This involves documenting all authorizations in a centralized location for easy access and tracking.
Staying organized with prior authorization requests
Implementing a robust documentation and record-keeping system can streamline the management of prior authorizations. Consider using spreadsheet software or cloud-based tools like pdfFiller to log details such as the date of submission, expected response times, and any follow-up actions needed.
Renewing or modifying authorizations
If there is a need to renew or modify an existing authorization—due to changes in treatment plans or the patient's condition—it's essential to follow the same structured approach used for initial submissions. Gather updated documentation, complete the form, and submit it following the previously discussed methods.
Interactive tools and resources
Online tools can significantly simplify the prior authorization process. Some providers offer a prior authorization search tool to enable users to check whether a service requires authorization and what specific criteria must be met.
Prior authorization search tool
Using your insurance company's prior authorization search tool can save time and provide clarity about the requirements for each service. Enter specific details about the procedure to quickly ascertain the necessary steps.
FAQs and troubleshooting common issues
Addressing common problems encountered during the process can enhance efficiency. Questions often arise concerning timeframes, approval processes, and appeals. Being proactive in seeking out the answers to these FAQs can prepare you for potential obstacles.
Conclusion: maximizing efficiency in your prior authorization process
The medical prior authorization process is a critical step in the healthcare delivery system, ensuring that patients receive appropriate treatments. Utilizing technology, such as pdfFiller, can significantly enhance efficiency in this process.
By leveraging streamlined editing, eSignature capabilities, and collaboration features, healthcare teams can focus more on patient care while minimizing administrative burdens. pdfFiller empowers users to seamlessly edit PDFs, eSign, collaborate, and manage documents from a single, cloud-based platform, helping to support a smooth authorization experience.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my medical prior authorization directly from Gmail?
How can I send medical prior authorization for eSignature?
Where do I find medical prior authorization?
What is medical prior authorization?
Who is required to file medical prior authorization?
How to fill out medical prior authorization?
What is the purpose of medical prior authorization?
What information must be reported on medical prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.