Get the free Multiple Sclerosis Agents Prior Authorization Form
Get, Create, Make and Sign multiple sclerosis agents prior



How to edit multiple sclerosis agents prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out multiple sclerosis agents prior

How to fill out multiple sclerosis agents prior
Who needs multiple sclerosis agents prior?
Multiple sclerosis agents prior form: A comprehensive guide
Understanding multiple sclerosis treatment options
Multiple sclerosis (MS) is a chronic autoimmune disorder that affects the central nervous system. The treatment landscape for MS primarily consists of disease-modifying therapies (DMTs), symptomatic treatments, and corticosteroids. Agents classified as DMTs, like interferons and monoclonal antibodies, are crucial in reducing the frequency of relapses and slowing disease progression.
Prior authorization has become increasingly important in the management of MS treatments, as it aims to ensure that patients receive appropriate therapies while controlling healthcare costs. Given that many agents used for MS require prior approval from insurance carriers, understanding the process is vital for patients and providers alike.
The role of prior authorization in MS treatment
Prior authorization is a process used by insurance companies to determine whether a specific treatment or medication is medically necessary. It plays a crucial role in controlling costs and ensuring that patients only receive treatments that are deemed appropriate based on their medical history and condition. For individuals with MS, securing prior authorization is essential for accessing the necessary medications.
The prior authorization process entails several steps, including submitting medical records and a detailed treatment plan. Key stakeholders involved typically include the patient, the prescribing physician, and the insurance provider. Effective communication among these parties is vital to minimize delays and secure timely approval for treatment.
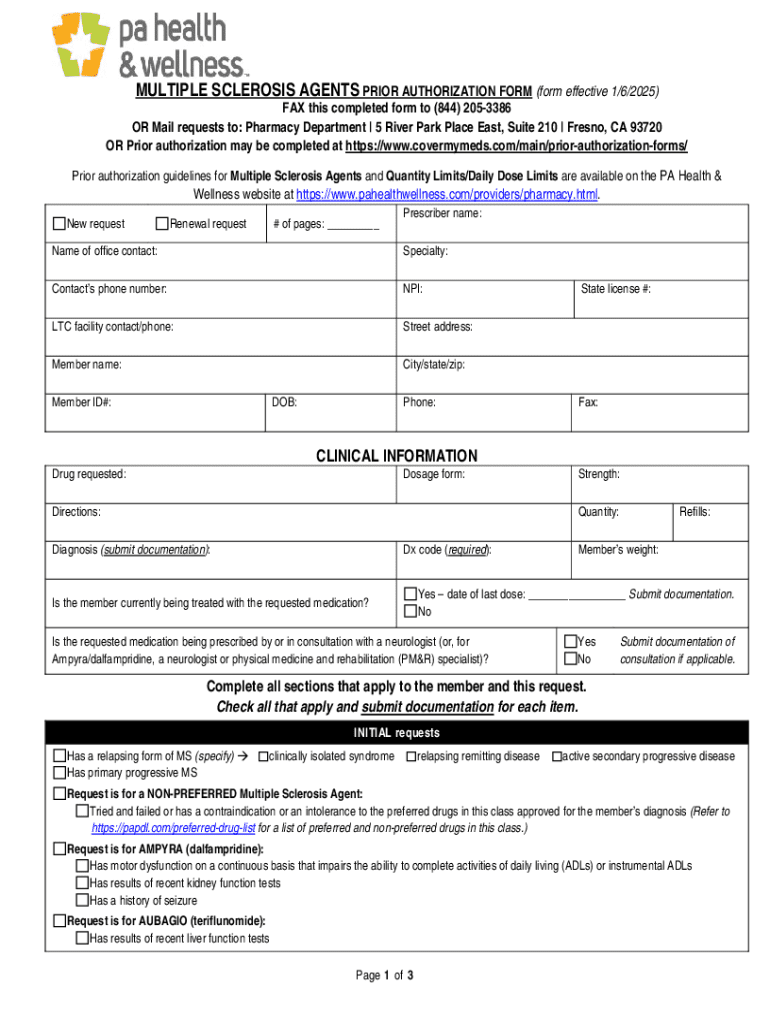
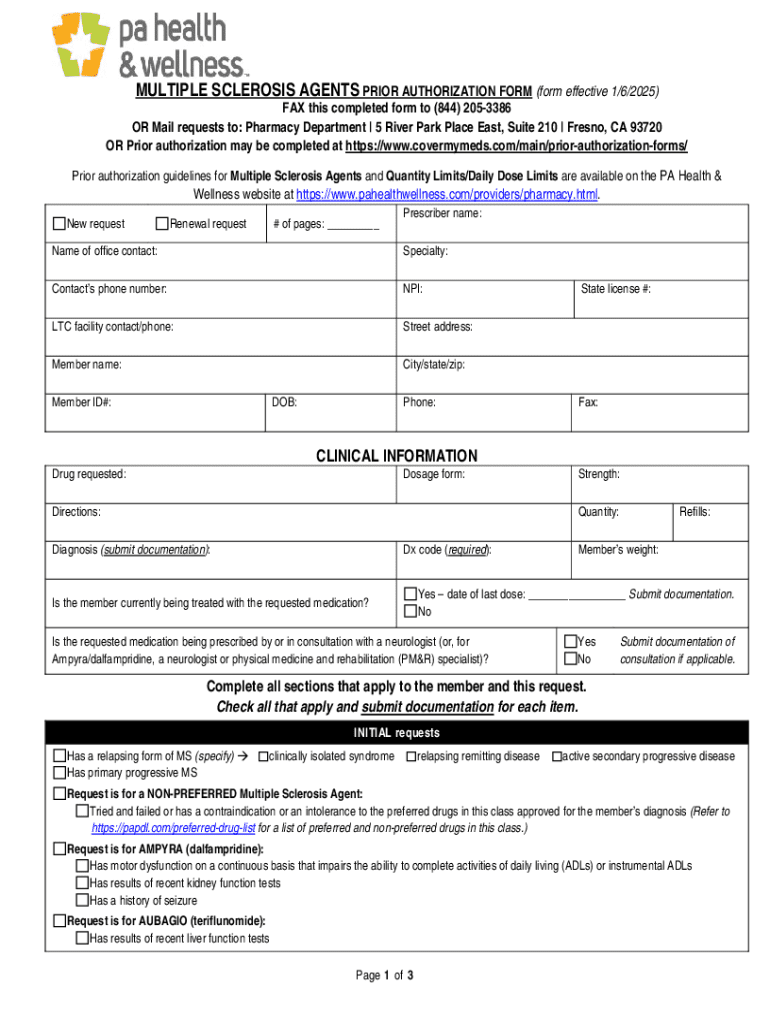
Preparing for the prior authorization submission
Before submitting a prior authorization form, it's essential to gather comprehensive patient information. This includes demographic details such as the patient's name, address, date of birth, and insurance information, as well as a thorough medical history that documents the diagnosis of MS and treatments received to date.
Diagnostic documentation, such as MRI results and clinical notes, is often required to provide context for the prescribing physician’s choice of therapy. Additionally, accurate prescription requirements, including the specific medication, dosage, and treatment duration, must be outlined in the submission.
The multiple sclerosis agents prior form
The prior authorization form itself has a particular structure that needs to be correctly filled out to ensure a successful submission. The form typically contains several sections, most importantly focused on patient information, medical necessity, and the prescribing physician's details.
Critical fields within the form include demographic data of the patient, the prescribing physician's credentials, and medication specifics, such as dosage and treatment rationale. Each section of the form serves a unique purpose in documenting the legitimacy of the treatment being requested.
Step-by-step instructions for filling out the form
Filling out the prior form requires attention to detail. Below is a step-by-step guide.
Interactive tools for enhanced navigation
Utilizing tools like pdfFiller can enhance the overall experience of navigating the prior forms. With pdfFiller’s document editing capabilities, healthcare providers and patients can fill out, edit, and securely manage forms.
The platform allows users to collaborate efficiently, enabling interactions between healthcare providers and patients. Storing documents securely in the cloud ensures that all parties have access to the most current versions of forms, making the submission process easier.
Common mistakes to avoid when completing the prior form
Errors on the prior authorization form can lead to significant delays in treatment. Common mistakes include leaving sections incomplete or failing to provide necessary documentation that supports the medical necessity of the prescribed treatment.
Misunderstandings regarding the authorization requirements can also result in resubmission. To prevent issues, it's crucial to double-check all details before submission, ensuring accuracy and completeness.
What to expect after submission
Once the prior authorization form is submitted, the waiting period begins. Typically, the insurance provider will process the request, and a response will be provided within a designated timeframe, which can vary based on the insurer's policies.
There are several potential outcomes following submission: the request may be approved, denied, or necessitate additional information. In cases of denial, it's vital to understand the reasons and to consider the appeal process, which usually requires additional documentation and a new justification for treatment.
Leveraging cloud-based solutions for document management
Cloud-based solutions have revolutionized how healthcare documentation is managed. Platforms like pdfFiller offer users the ability to store and edit documents securely, access them from anywhere, and track their status in real-time.
The integration of electronic signatures streamlines the process by eliminating the need for physical paperwork. Such efficiency not only saves time but also ensures that all documents remain accessible for future reference, thus facilitating smoother interactions with healthcare providers.
FAQs about multiple sclerosis agents prior forms
Frequently asked questions surrounding the prior authorization process can help clarify concerns. Common queries include reasons for prior authorization delays, potential alternatives to medications requiring authorization, and how pdfFiller can assist in alleviating unnecessary paperwork.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make edits in multiple sclerosis agents prior without leaving Chrome?
Can I edit multiple sclerosis agents prior on an iOS device?
How do I fill out multiple sclerosis agents prior on an Android device?
What is multiple sclerosis agents prior?
Who is required to file multiple sclerosis agents prior?
How to fill out multiple sclerosis agents prior?
What is the purpose of multiple sclerosis agents prior?
What information must be reported on multiple sclerosis agents prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.