Get the free Medication Prior Authorization Request Form
Get, Create, Make and Sign medication prior authorization request



Editing medication prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medication prior authorization request

How to fill out medication prior authorization request
Who needs medication prior authorization request?
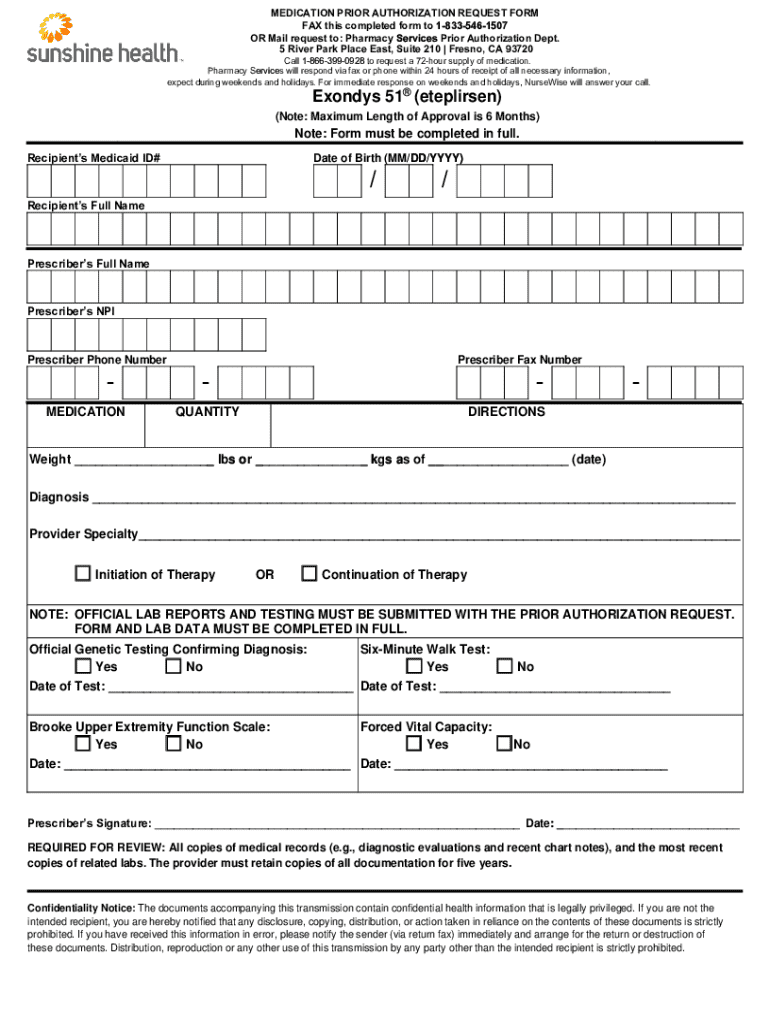
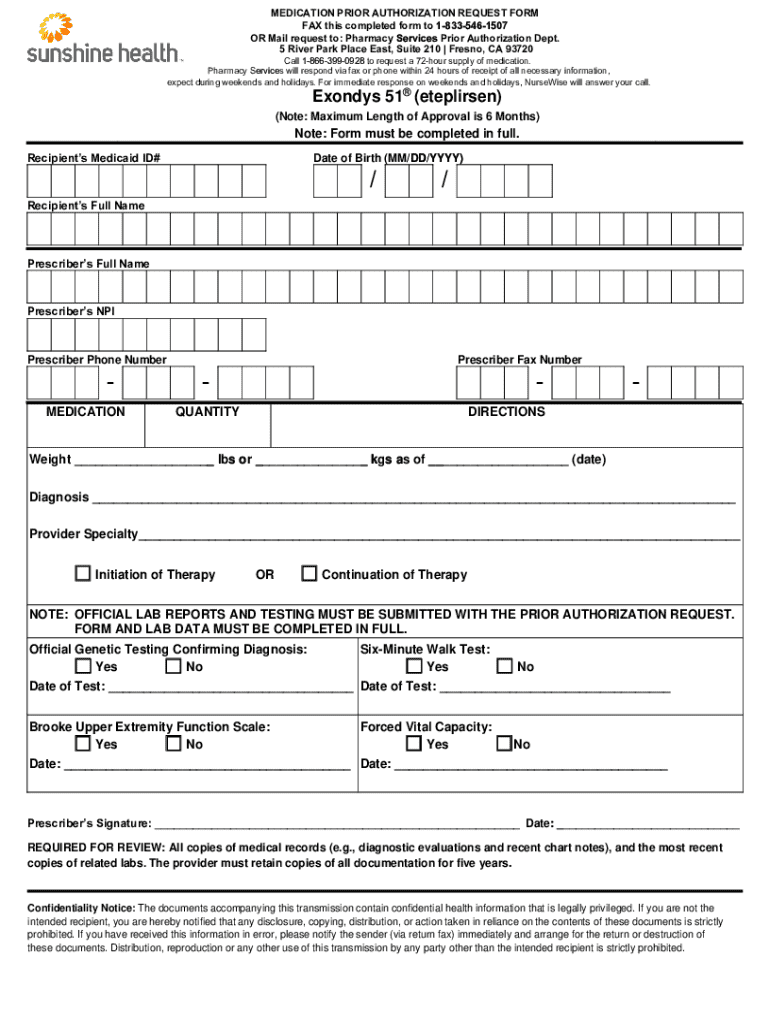
Medication Prior Authorization Request Form: Detailed Guide
Understanding the medication prior authorization process
Prior authorization is a process required by many insurance providers to ensure that certain medications or treatments are appropriately vetted before being approved for payment. It serves as a way to verify that the prescribed treatment is medically necessary based on the patient's specific health circumstances. Essentially, prior authorization acts as a check and balance in the healthcare system, preventing potentially unnecessary or excessively costly treatments.
The necessity of prior authorization often arises in response to the soaring costs of healthcare and medications. By ensuring that patients receive only what is appropriate, healthcare providers can help minimize overall expenses.
Common medications requiring authorization
Certain classes of medications are more likely to require prior authorization due to their high costs or the complexity of their usage. For instance, specialty medications, which are often used to treat complex or chronic illnesses, frequently fall under this category.
Examples of common categories of medications requiring authorization include: Antineoplastics for cancer treatment, biologics for autoimmune disorders, and opioids in pain management. Healthcare providers must check each medication's eligibility under an insurance plan to avoid any payment surprises for their patients.
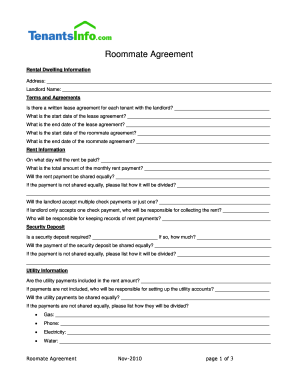
Components of the medication prior authorization request form
A medication prior authorization request form typically includes several key components that provide essential information to both the insurer and the healthcare provider. Filling out every component accurately is crucial for the approval process.
Key information required on the form consists of:
Additionally, providing supplemental documentation like clinical notes, evidence of previous treatments, and the patient’s medical history can significantly bolster the case for approval.
Step-by-step instructions for completing the form
Completing the medication prior authorization request form can be straightforward if you follow a structured approach. Here's a step-by-step guide:
First, prepare to fill out the form by gathering all necessary documents and verifying patient and medication details. This ensures that you have all the pertinent information at your fingertips.
Finally, double-check everything for accuracy. Careful review can prevent costly delays in processing the prior authorization request.
Interactive tools and features on pdfFiller
pdfFiller enhances the process of completing the medication prior authorization request form through its useful cloud-based features. Having access to your documents from anywhere, at any time, means you can work on the form whenever necessary.
The platform also offers a variety of easy editing tools for PDFs, ensuring that adding, removing, or changing information is a breeze.
Submitting the medication prior authorization request
Submitting your medication prior authorization request can vary based on your organization's protocols. Generally, there are two main submission options: electronic and paper.
Electronic submissions are often quicker and may feature built-in tracking mechanisms, while paper submissions may require more time to process.
Tips for ensuring a successful prior authorization approval
To enhance the chances of obtaining prior authorization approval, it is crucial to understand the specifics of insurance policies.
Researching individual insurer requirements can be invaluable in avoiding common pitfalls. Knowing the reasons claims are frequently denied allows providers to craft more compelling justifications for treatment.
What to do if your prior authorization is denied
Receiving a denial can be discouraging, but it is important to carefully review the denial notice. Crucial elements, such as the reason for the denial and any guidance on how to appeal, can be found in this notice.
Follow these steps to effectively navigate a denial situation:
Utilizing pdfFiller for ongoing document management
Managing documents, especially those related to medication prior authorization requests, can become overwhelming without an organized method. pdfFiller offers solutions for keeping records organized and accessible.
Using pdfFiller's folders and tagging systems allows individuals and teams to retrieve documents quickly. Collaboration features further help streamline the communication process among healthcare teams.
Frequently asked questions (FAQs)
Understanding the medication prior authorization request form can generate various questions and concerns, especially for those unfamiliar with the process. Below are some common inquiries:
These FAQs address significant concerns and can guide users in navigating the process more efficiently.
Glossary of key terms related to medication prior authorization
Familiarizing yourself with key terms utilized in the medication prior authorization process is essential for effective communication with insurers and understanding the process. Below are important terms:






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my medication prior authorization request in Gmail?
How can I modify medication prior authorization request without leaving Google Drive?
Can I create an eSignature for the medication prior authorization request in Gmail?
What is medication prior authorization request?
Who is required to file medication prior authorization request?
How to fill out medication prior authorization request?
What is the purpose of medication prior authorization request?
What information must be reported on medication prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.