Get the free Standard Prior Authorization Request Form
Get, Create, Make and Sign standard prior authorization request



Editing standard prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out standard prior authorization request

How to fill out standard prior authorization request
Who needs standard prior authorization request?
Understanding the Standard Prior Authorization Request Form
Understanding the standard prior authorization process
Prior authorization (PA) is a crucial step in the healthcare process, ensuring that patients receive necessary medical interventions while controlling costs for insurers. This process requires healthcare providers to obtain approval from a patient's health plan before delivering specific services, medications, or procedures.
The importance of prior authorization cannot be overstated. It serves as a cost-containment measure, helping to prevent unnecessary treatments, reduce fraud, and optimize patient care. This is especially relevant in healthcare systems strained by rising costs and limited resources. Without prior approval, providers risk incurring costs that may not be reimbursed by insurers.
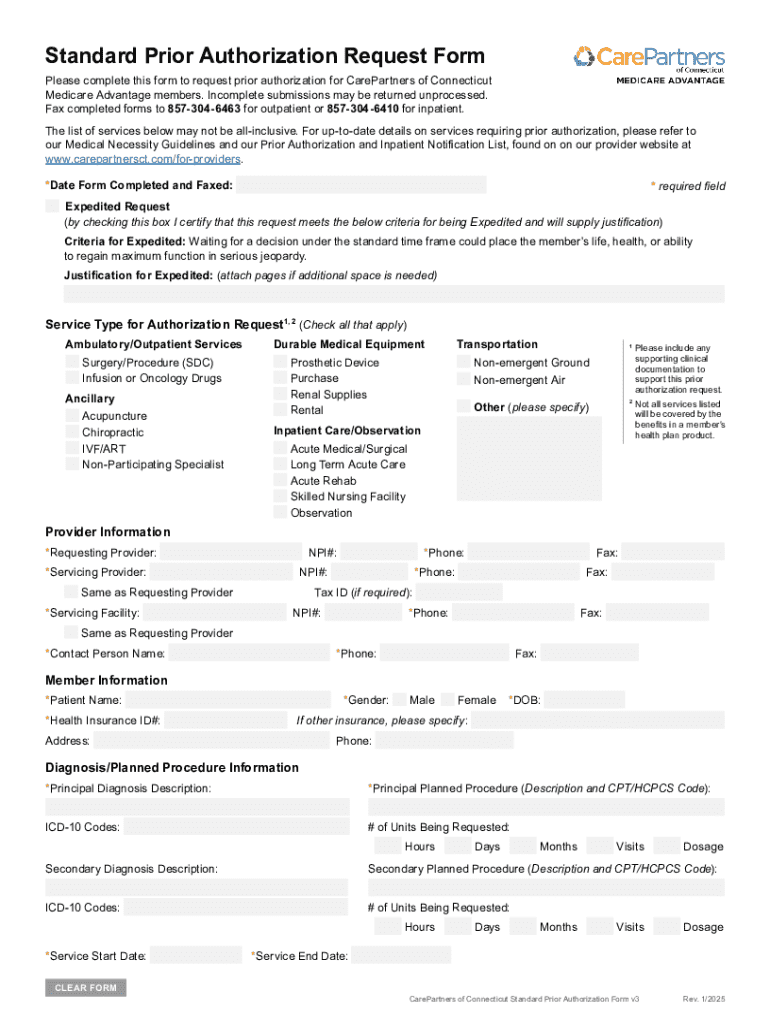
Key components of a standard prior authorization request form
A standard prior authorization request form is carefully structured to capture essential information that facilitates the approval process. Each component is crucial for a successful submission, enabling insurers to evaluate the necessity of the requested service effectively.
Patient information is the first section and typically includes demographics such as name, date of birth, and insurance details, enabling the insurer to verify coverage. Next is the provider information, where details about the referring provider, their specialties, and contact information must be listed accurately.
The service details section covers what is being requested, including the type of service, medical necessity information, and any supporting documentation that may be required by the insurer to substantiate the request.
Step-by-step guide to completing the standard prior authorization request form
Completing a standard prior authorization request form may seem daunting, but breaking it down into manageable steps can simplify the process significantly. The aim is to ensure accuracy and comprehensiveness.
Step 1 involves gathering necessary documents, including the patient's medical history, previous treatment records, and lab results. These will support your request for services or medications.
In Step 2, it's essential to fill out patient information accurately to avoid any delays. This includes verifying all demographics and insurance plans.
Step 3 focuses on providing comprehensive provider information, ensuring that all details regarding the referring provider's practice and specialties are correct. In Step 4, service details should be clearly specified, including the codes using CPT/HCPCS as required.
For Step 5, it's important to justify medical necessity convincingly. Utilize clinical data and previous treatment responses to illustrate why the service is required. Finally, in Step 6, review the entire submission, ensuring all information is complete and accurate.
Common mistakes to avoid when submitting prior authorization requests
Submitting a prior authorization request is not without its challenges. Understanding common pitfalls can dramatically improve success rates. One frequent issue is incomplete forms. Failure to fill out all required sections could lead to automatic denials, wasting valuable time.
Another common mistake is the absence of supporting documentation. Insurers need evidence to support every request, and without it, approval is highly unlikely. Additionally, incorrect coding or misinformation can significantly delay the process and lead to rejections.
Tips for efficiently managing prior authorization requests
Efficiently managing prior authorization requests is fundamental to maintaining operational flow in a healthcare practice. Leveraging technology, such as pdfFiller's document creation and management tools can significantly streamline the process.
Establishing a tracking system for all requests helps ensure no submissions are overlooked. Furthermore, creating communication channels with insurers can aid in clarifying requirements or resolving any issues promptly, reducing the chances of errors.
Navigating the challenges of prior authorization
The process of prior authorization can be fraught with challenges, both for healthcare providers and patients. Common issues include delays in approval, insufficient information requests, and outright denials. Understanding these challenges is the first step toward mitigating them.
Providers can devise strategies to overcome such hurdles by keeping detailed records of all communications and consistently following up on pending requests. Persistence can pay off, especially when clarifying cases that appear to be stalled or denied.
Leveraging pdfFiller for your standard prior authorization needs
pdfFiller offers powerful interactive tools designed for managing standard prior authorization request forms effectively. Users can fill out forms seamlessly, thanks to intuitive design features. The platform supports eSignature capabilities, allowing for swift approvals, which is crucial in urgent healthcare situations.
Collaboration becomes easy with pdfFiller, enabling team members to work together on forms. Furthermore, the cloud-based nature of the platform allows users to access forms anytime and anywhere, ensuring flexibility and efficiency in managing request submissions.
Frequently asked questions about the prior authorization process
Understanding the prior authorization process thoroughly helps patients and providers navigate potential uncertainties. A common question is what to do if a request is denied. In most cases, providers can appeal the denial by providing additional evidence or clarification regarding medical necessity.
Another frequently asked question is the duration of the prior authorization process. Generally, it can take anywhere from a few days to several weeks, depending on the complexity of the request and the responsiveness of the insurer. Patients often wonder if they can expedite a prior authorization request; some insurance companies allow this under specific circumstances, usually where urgent care is needed.
Best practices for healthcare providers regarding prior authorizations
Establishing a standard process for submitting prior authorizations can greatly benefit healthcare providers. Having clear guidelines ensures that all staff members are informed of procedures, reducing errors and improving efficiency.
Training staff on submission requirements is also crucial since the prior authorization process can vary significantly from one insurer to another. Providers should prioritize staying informed about any payer-specific guidelines and updates to ensure compliance.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my standard prior authorization request in Gmail?
Can I sign the standard prior authorization request electronically in Chrome?
How do I fill out standard prior authorization request using my mobile device?
What is standard prior authorization request?
Who is required to file standard prior authorization request?
How to fill out standard prior authorization request?
What is the purpose of standard prior authorization request?
What information must be reported on standard prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.