Get the free Nc Medicaid Pharmacy Prior Approval Request for Glp-1’s for Weight Management
Get, Create, Make and Sign nc medicaid pharmacy prior



Editing nc medicaid pharmacy prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nc medicaid pharmacy prior

How to fill out nc medicaid pharmacy prior
Who needs nc medicaid pharmacy prior?
NC Medicaid Pharmacy Prior Form: A Comprehensive How-To Guide
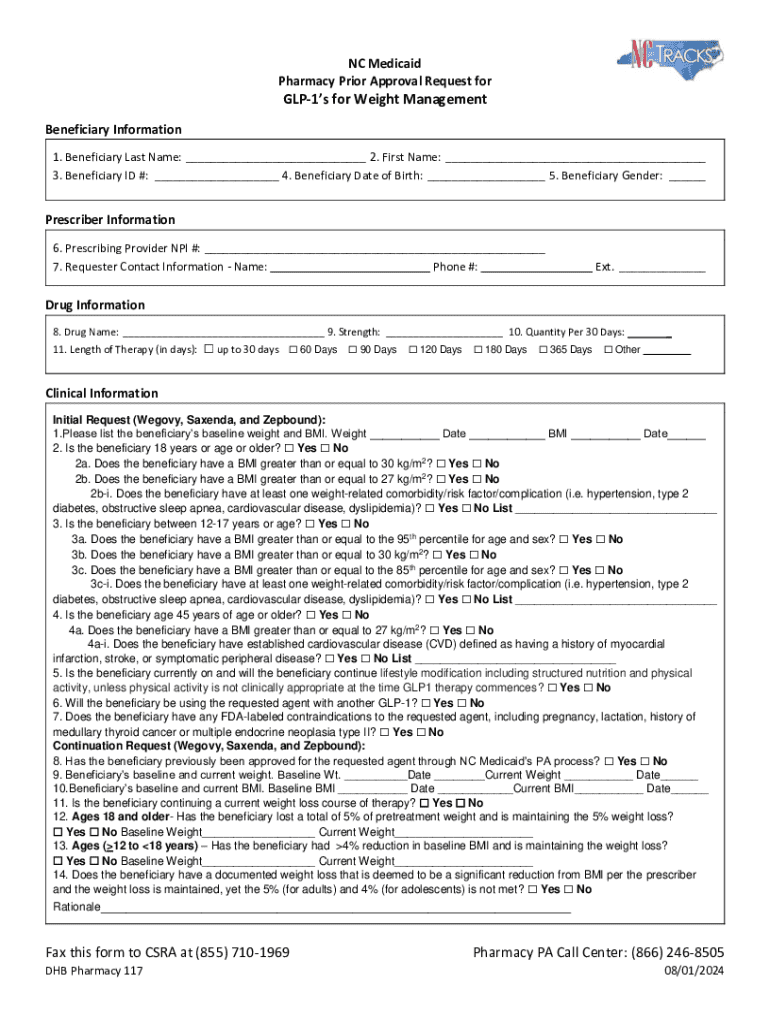
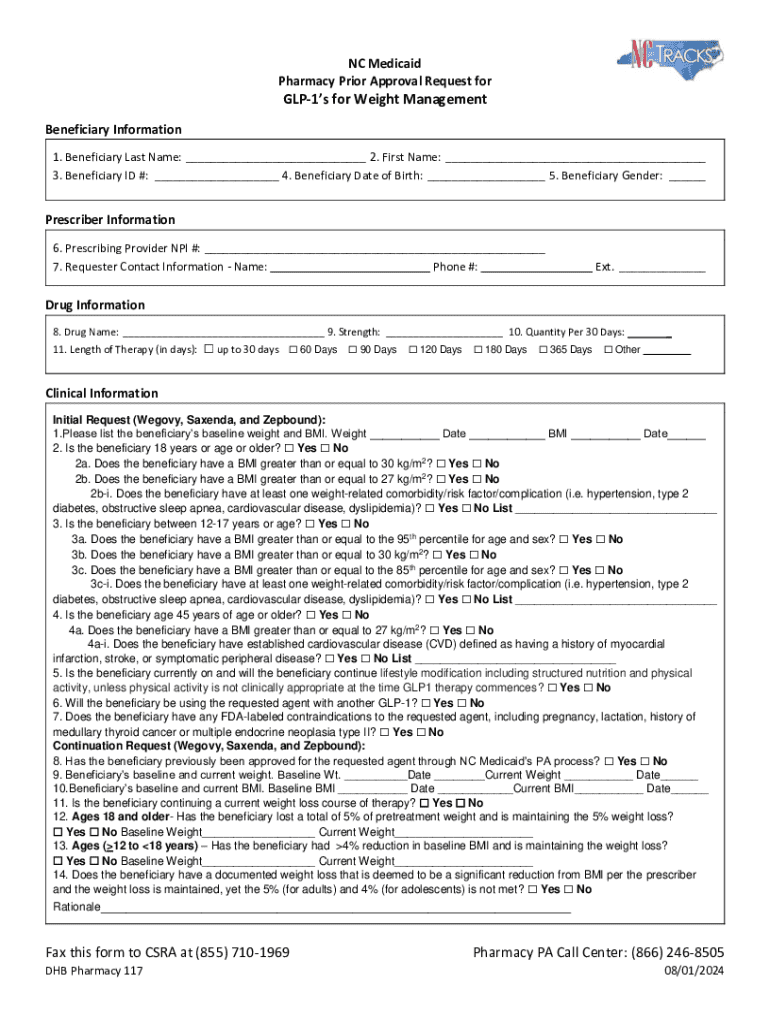
Understanding NC Medicaid Pharmacy Prior Authorization
NC Medicaid Pharmacy Prior Authorization is a critical component in managing medication access for recipients in North Carolina. This process is designed to ensure that medications prescribed to Medicaid members are necessary, appropriate, and covered by the Medicaid program. The importance of this authorization lies in its ability to prevent overutilization of medications, ensure cost-effectiveness, and enhance patient safety.
The prior authorization process for pharmacy services in NC Medicaid involves several steps, starting from a provider’s request to the assessment and determination made by the North Carolina Medicaid program. It serves as an additional safeguard to ensure that both providers and patients are making informed decisions about therapies that are medically appropriate.
Who needs to fill out the NC Medicaid Pharmacy Prior Form?
The NC Medicaid Pharmacy Prior Form is essential for various stakeholders in the Medicaid ecosystem, particularly members and healthcare providers. Medicaid members looking to obtain certain medications must have their healthcare providers submit requests on their behalf, primarily when those medications require prior approval.
Eligibility criteria for members include being enrolled in NC Medicaid and requiring medications that are classified as non-formulary or subject to restrictions. Providers play a crucial role in this process, as they must be well-versed in identifying which conditions and medications necessitate the prior authorization.
Step-by-step guide to completing the NC Medicaid Pharmacy Prior Form
Completing the NC Medicaid Pharmacy Prior Form accurately is crucial for a smooth authorization process. This section offers a detailed breakdown of how to effectively prepare for and fill out the form.
Preparing to fill out the form
Before beginning the form, gather necessary documents, including member identification, prescription information, and clinical justifications. Access the NC Medicaid Pharmacy Prior Form via the official NC Medicaid website. Download and print the form or utilize pdfFiller to fill it out digitally, enhancing ease of use.
Filling out the form
The NC Medicaid Pharmacy Prior Form consists of several sections that require specific information. Be sure to accurately fill out details such as patient information, medication details, prescribing provider information, and justifications. Common mistakes include incomplete sections, inaccurate medication codes, and lack of supporting documentation.
Submitting the form
After completion, the form can be submitted through various channels. Options include online submission via the NC Medicaid website, mailing it to the designated Medicaid office, or faxing it directly. Be mindful of key submission dates and deadlines to ensure timely processing.
Tracking your submission status
Once submitted, you can confirm receipt of your form through the provider portal or by contacting your local Medicaid office. Understanding response times is essential, as this can vary based on medication complexity, so follow-up is crucial.
Tips for successful prior authorization
One of the best ways to increase the success rate of your prior authorization request is to ensure accuracy. Double-checking your information before submission can prevent unnecessary delays. Additionally, crafting effective justifications is key—articulating why a medication is necessary can enhance your case for approval.
Utilizing tools like pdfFiller can dramatically simplify the document management process, enabling easy editing, signing, and collaboration. This allows you to focus on providing patient care rather than getting bogged down in paperwork.
Special considerations and exceptions
In certain situations, such as emergencies, expedited prior authorization requests can be initiated. Healthcare providers must clearly indicate the urgency when submitting the form. Pediatric cases may also have unique guidelines that necessitate consideration of age-related factors in medication dosage and necessity.
Understanding the denial process is critical. In the event of a denial, providers and members should be aware of their options, including the appeal process, which allows for a resubmission with additional documentation if needed.
Frequently asked questions (FAQ) about NC Medicaid pharmacy prior authorization
Several common inquiries arise regarding the NC Medicaid Pharmacy Prior Authorization process. Recipients often want to know about eligibility, the typical timeframe for approvals, and how to appeal a denial. Providers, on the other hand, seek clarification on documentation requirements and reimbursement policies.
Navigating regional operations and support
North Carolina Medicaid operates with regional variations, influencing how prior authorizations are processed. It’s essential to familiarize yourself with the specific protocols applicable to your region. Local resources for assistance include Medicaid offices and community health programs, which can provide valuable guidance.
Contacting your local Medicaid office can be a vital step for personalized support, especially for unique cases that may deviate from standard guidelines.
Additional information and tools for managing your documentation
Utilizing pdfFiller’s advanced features can streamline the document creation and management process for prior authorizations. Tools such as e-signatures and secure cloud storage mean that once you fill out the NC Medicaid Pharmacy Prior Form, you can edit and store it safely for future reference.
Effective collaboration with healthcare teams is also essential. Sharing documents securely and tracking changes ensures that all stakeholders are on the same page regarding a patient’s treatment plan.
Feedback and support
Providing feedback on your experience with the NC Medicaid Pharmacy Prior Authorization process contributes to ongoing improvements. Members and providers are encouraged to share their thoughts, which help refine workflows and documentation practices. For those requiring language assistance or auxiliary aids, resources are available through the Medicaid office.
Should you encounter challenges or have specific questions, reaching out via the provided contact methods can help clarify concerns and guide you further.
Login and access information
Members and providers can access their accounts through the NC Medicaid member and provider portals. Ensure that you have the necessary credentials for smooth access. If you experience login issues, solutions often involve recovering your username or resetting your password through the portal’s support feature.
Quick links to tailored plan services and information
The NC Medicaid website offers a range of programs and services directly related to pharmacy authorization. Quick links to forms and resources related to medication management can greatly assist members and providers in navigating the system efficiently.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an eSignature for the nc medicaid pharmacy prior in Gmail?
How do I fill out the nc medicaid pharmacy prior form on my smartphone?
Can I edit nc medicaid pharmacy prior on an Android device?
What is nc medicaid pharmacy prior?
Who is required to file nc medicaid pharmacy prior?
How to fill out nc medicaid pharmacy prior?
What is the purpose of nc medicaid pharmacy prior?
What information must be reported on nc medicaid pharmacy prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.