Get the free Prior Authorization Request
Get, Create, Make and Sign prior authorization request
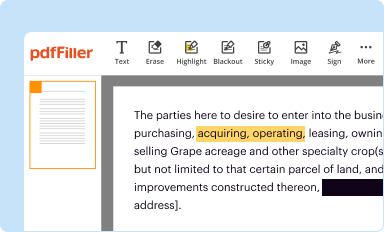
How to edit prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request
How to fill out prior authorization request
Who needs prior authorization request?
Prior Authorization Request Form: A Comprehensive How-to Guide
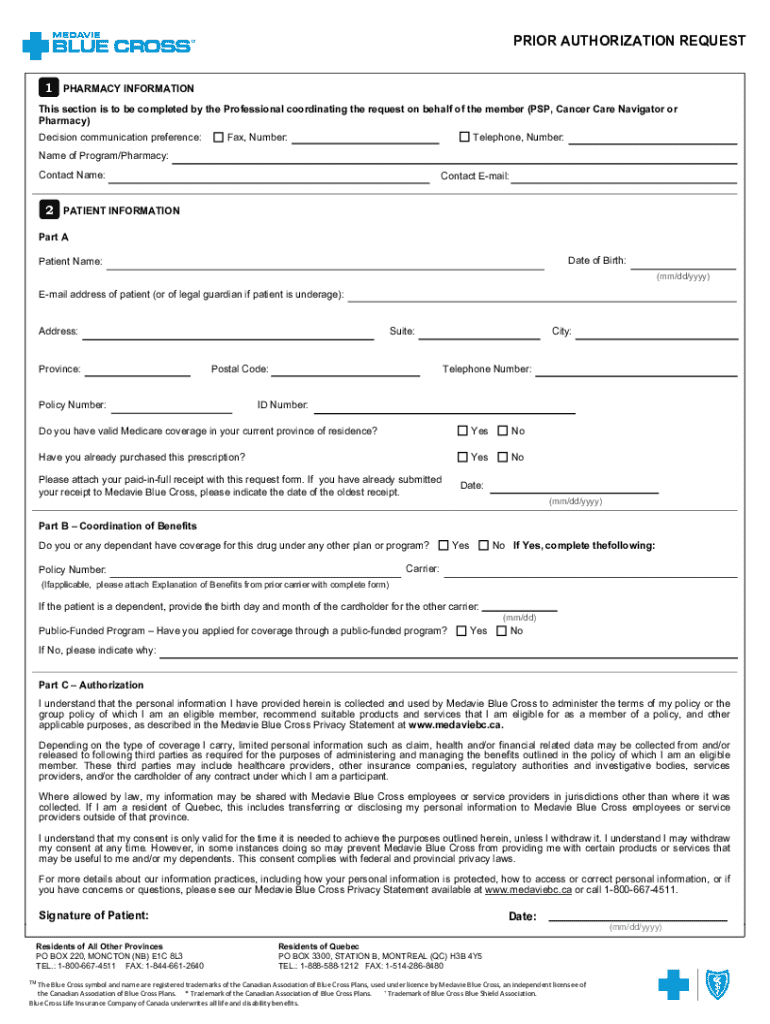
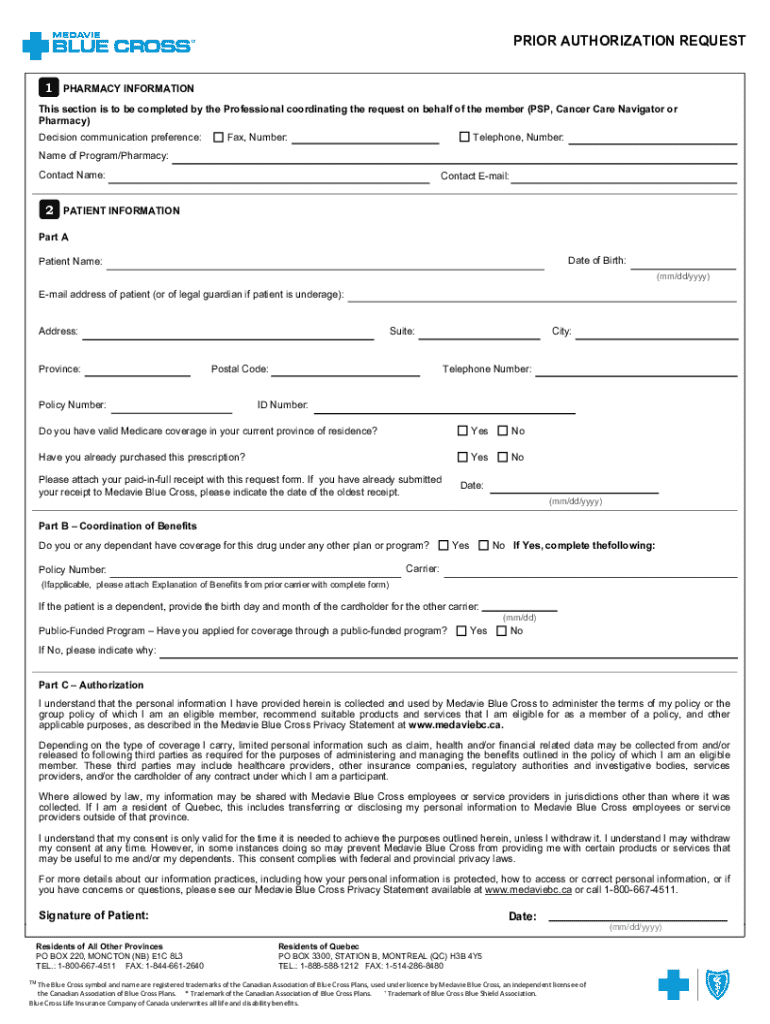
Understanding the prior authorization request form
A prior authorization request form is an essential document in healthcare that serves as a formal request from a healthcare provider to an insurance company for approval of a particular treatment, medication, or test. This process is crucial because it helps ensure that treatments align with patient care protocols and coverage rules, preventing unnecessary costs for both patients and providers.
Components of the prior authorization request form
Completing a prior authorization request form correctly involves gathering various components. Each section plays a pivotal role in communicating necessary details for the approval process.
Essential information includes:
In addition to these components, submitting supporting documentation such as clinical notes, lab results, and previous treatment responses can improve the chances of approval.
Steps to complete the prior authorization request form
Completing the prior authorization request form can seem daunting, but breaking it down into manageable steps simplifies the process significantly.
Best practices for submitting prior authorization requests
To streamline the prior authorization process, implementing best practices can significantly enhance efficiency.
Challenges and solutions in the prior authorization process
The prior authorization process is not without its challenges. Common issues include prolonged processing times, denials for insufficient information, and the overall complexity of the forms.
To tackle these issues effectively, consider the following strategies:
Impact of prior authorization on patient care
The effectiveness of patient care can be severely impacted by delays in prior authorization approval. Studies have shown that patients often experience longer waiting periods for necessary treatments due to these bureaucratic hurdles.
Without timely approvals, patients may delay treatment, worsening their health conditions and increasing the overall costs on acute care scenarios. Testimonials from healthcare providers emphasize the stress caused by frantic attempts to manage authorization requests while ensuring quality care.
Legal and compliance considerations
Understanding the compliance aspects of the prior authorization request is essential for healthcare providers. Regulations such as HIPAA dictate the confidentiality of patient information.
Proper documentation is not only necessary for facilitating patient care but also crucial for avoiding compliance issues. Best practices include maintaining stringent records of all transactions and safeguarding patient data.
Future trends in prior authorization
The prior authorization landscape is gradually changing, thanks to technological advancements. Automation and artificial intelligence are paving the way for more expedient handling of requests.
We can anticipate changes in policies that will streamline practices even further, reducing administrative burdens on healthcare providers and enhancing patient experience.
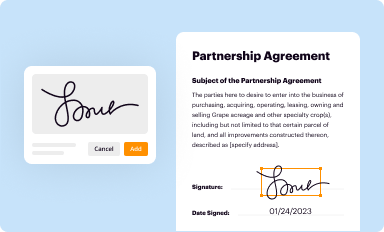
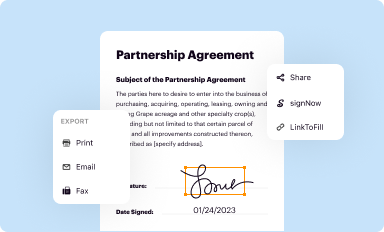
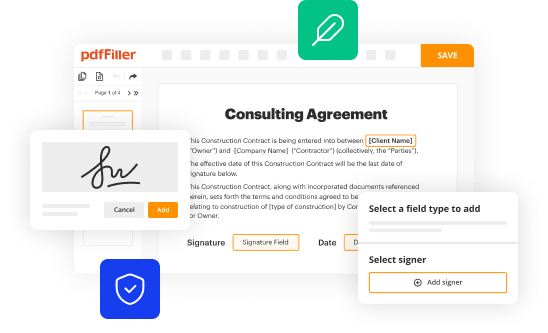
Utilizing pdfFiller in the prior authorization process
pdfFiller provides an invaluable platform for users managing prior authorization request forms. It simplifies the editing, signing, and submitting process, making it accessible to individuals and teams alike.
Key features include:
Conclusion
Navigating the complexities of the prior authorization request form doesn’t have to be overwhelming. By following the detailed steps outlined in this guide, healthcare providers and teams can improve efficiency, reduce errors, and ultimately enhance patient care.
Implementing tools like pdfFiller can further streamline the process, providing a comprehensive solution for managing important healthcare documents.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I sign the prior authorization request electronically in Chrome?
How do I fill out the prior authorization request form on my smartphone?
How do I edit prior authorization request on an Android device?
What is prior authorization request?
Who is required to file prior authorization request?
How to fill out prior authorization request?
What is the purpose of prior authorization request?
What information must be reported on prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.