Get the free Kaiser Permanente Prior Authorization
Get, Create, Make and Sign kaiser permanente prior authorization
Editing kaiser permanente prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out kaiser permanente prior authorization
How to fill out kaiser permanente prior authorization
Who needs kaiser permanente prior authorization?
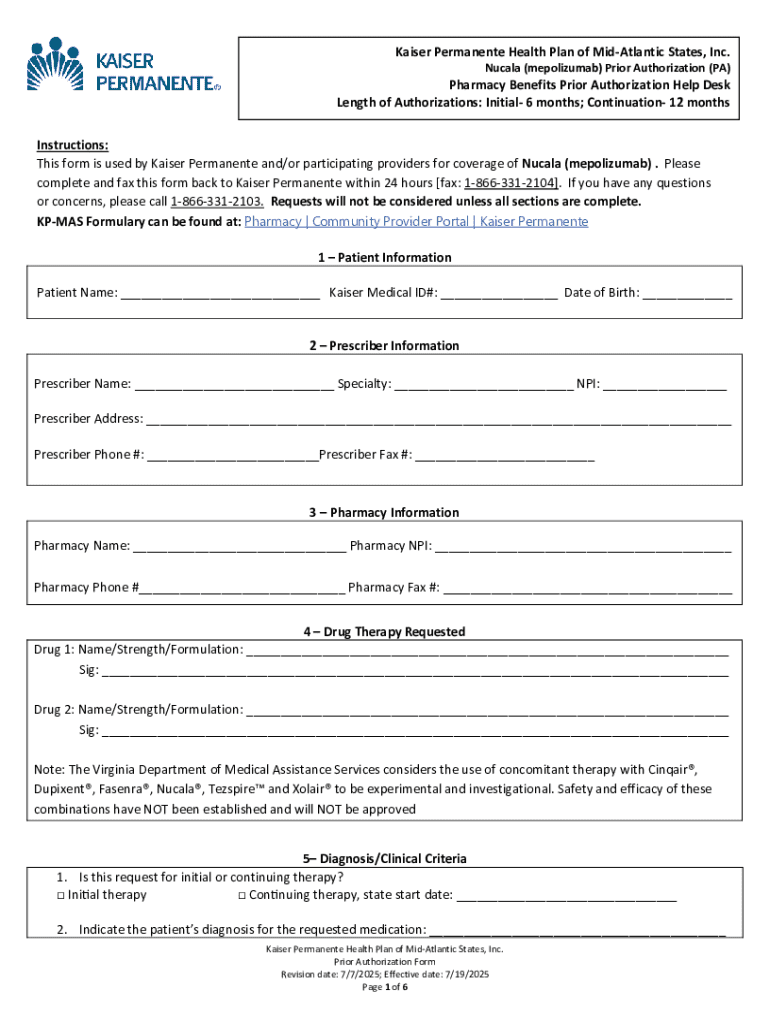
Kaiser Permanente Prior Authorization Form – How-to Guide
Understanding prior authorization
Prior authorization is a critical process in the healthcare system that serves as a hurdle that healthcare providers must clear before certain treatments or tests can be administered to patients. This mechanism ensures that the services requested align with medical necessity and that they meet the clinical guidelines set forth by insurers like Kaiser Permanente. Essentially, prior authorization functions to control healthcare costs and streamline insurance claims processing.
Insurance companies, including Kaiser Permanente, require prior authorization to determine whether the proposed service or medication is appropriate based on the patient's specific health situation. This not only helps in managing costs but also helps maintain a standard of care that is necessary for optimal patient outcomes.
Key components of the Kaiser Permanente prior authorization form
The Kaiser Permanente prior authorization form is divided into several essential sections, each aimed at collecting specific data necessary for processing the authorization request effectively. Understanding these components is crucial for anyone tasked with filling out this document.
Additionally, the form utilizes technical terms such as CPT (Current Procedural Terminology) codes and diagnosis codes which are critical for accurately processing the request. Familiarity with these terms can significantly reduce errors and streamline the process.
Step-by-step guide to completing the authorization form
Completing the Kaiser Permanente prior authorization form can be straightforward if you have all the necessary information at hand. Follow this step-by-step guide to ensure you fill out the form accurately.
Start by gathering essential documents such as the patient's medical history, previous treatment plans, and any previous authorizations that can support the current request. This information is vital as it provides context for the request, which is necessary for a thorough review.
Once the form is filled out, you will need to submit it either electronically through the Kaiser Permanente online portal or in hard copy via mail. Confirm the appropriate submission method based on the urgency of the request and any specific instructions provided by the patient's health plan.
Managing your submission
After submitting the Kaiser Permanente prior authorization form, it is crucial to track your request effectively. Kaiser Permanente offers online tools for members or providers to check the status of their submissions. This feature allows for peace of mind while waiting for decisions.
Expect to receive a decision on your authorization request within a stipulated time frame, often communicated once you submit the form. Common outcomes include approval, denial, or requests for additional information, which can prolong the process.
Understanding the review process
The review process for prior authorizations at Kaiser Permanente is thorough, involving peer reviewers who assess the medical necessity of the requested services based on established clinical guidelines. Criteria such as the severity of the condition, prior treatment attempts, and outcomes play a significant role in shaping the review outcome.
Challenges may arise during the review process, particularly if the information provided is insufficient or unclear. Common reasons for denial include lack of evidence supporting medical necessity or failure to provide all required documentation. Understanding these challenges can help in ensuring a successful authorization request.
Handling denials and appeals
Receiving a denial from Kaiser Permanente can be disheartening, but it is not the end of the road. Understanding how to interpret denial letters is essential for successfully managing the appeal process. The letter will typically outline the reasons for denial, which can guide you in addressing the issues raised.
When filing an appeal, be thorough, clear, and organized. This approach increases the chances of a successful resolution, and including any additional medical evidence can bolster your case significantly.
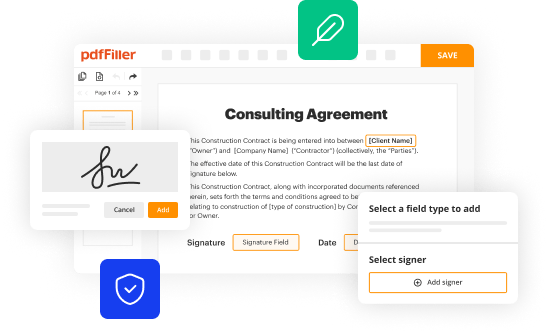
Utilizing pdfFiller for the Kaiser Permanente prior authorization form
Using pdfFiller can significantly simplify the process of completing the Kaiser Permanente prior authorization form. This platform provides users with the tools needed for seamless editing and formatting of PDFs, ensuring that all necessary information is included.
These features make pdfFiller an invaluable ally in managing the authorization process efficiently and effectively.
Frequently asked questions
As you navigate the prior authorization landscape, you might encounter several common queries about the process. Understanding these can help clear up any confusion and set realistic expectations.
Additionally, if you face challenges while using pdfFiller, technical support is available to assist with accessing or filling out forms, ensuring that the submission process goes as smoothly as possible.
Best practices for future requests
To enhance efficiency when submitting future prior authorization requests, it’s paramount to maintain thorough documentation. Keep records of all communications with insurance representatives and copies of submitted forms, as these can be crucial in situations where clarification is needed.
Being proactive about these practices can significantly reduce misunderstandings and streamline future requests.
Final tips for success
Success in navigating the Kaiser Permanente prior authorization form hinges on one primary factor: accuracy. Double-checking all entries before submission is essential to avoid common pitfalls that can lead to delays or denials.
With this guide, individuals and teams can empower themselves to navigate the Kaiser Permanente prior authorization form effectively, leveraging pdfFiller's cloud-based solution for enhanced document management.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit kaiser permanente prior authorization from Google Drive?
How do I make changes in kaiser permanente prior authorization?
How do I complete kaiser permanente prior authorization on an Android device?
What is kaiser permanente prior authorization?
Who is required to file kaiser permanente prior authorization?
How to fill out kaiser permanente prior authorization?
What is the purpose of kaiser permanente prior authorization?
What information must be reported on kaiser permanente prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.