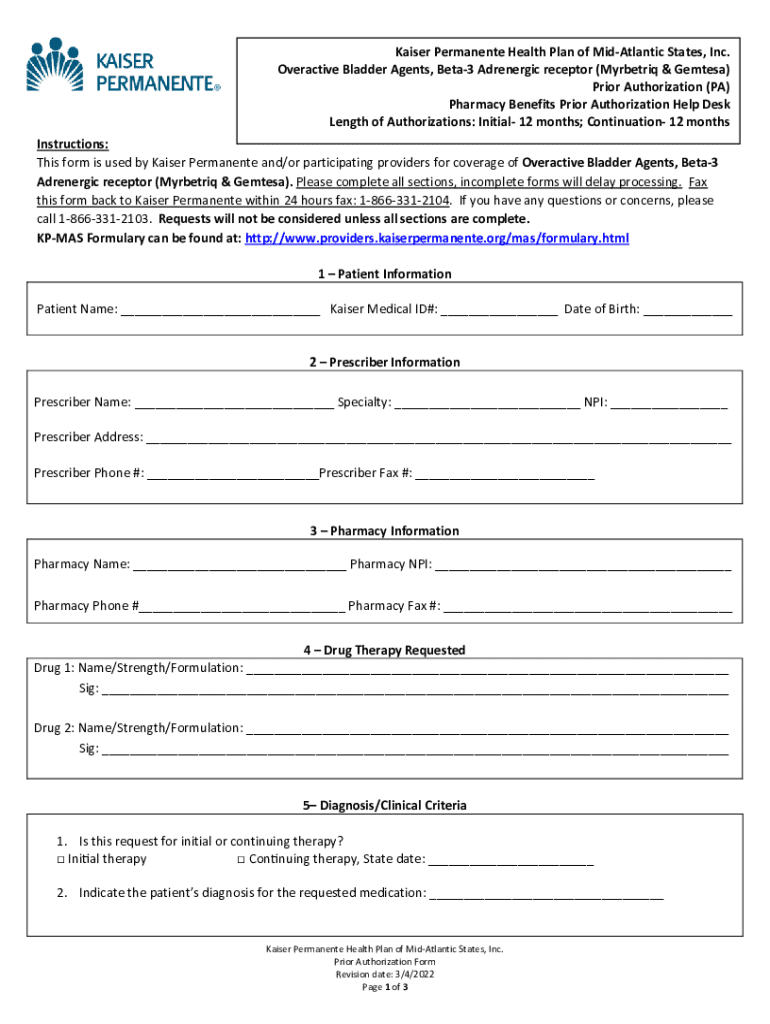
Get the free Kaiser Permanente Prior Authorization Form
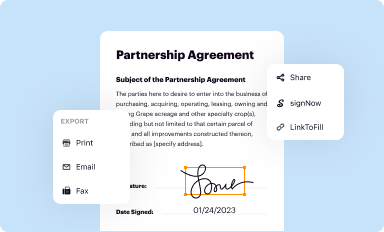
Get, Create, Make and Sign kaiser permanente prior authorization
How to edit kaiser permanente prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out kaiser permanente prior authorization
How to fill out kaiser permanente prior authorization
Who needs kaiser permanente prior authorization?
Kaiser Permanente Prior Authorization Form: A Comprehensive How-to Guide
Understanding the Kaiser Permanente Prior Authorization Process
Prior authorization is a vital step in the healthcare delivery process that requires healthcare providers to obtain approval from a health insurance company before delivering specific services or medications. The purpose of prior authorization is to manage costs and ensure that the prescribed treatment is medically necessary. This process is crucial for both patients and providers as it plays a significant role in the healthcare system, preventing unnecessary treatments and keeping healthcare costs manageable.
The importance of prior authorization cannot be overstated. It safeguards patients against receiving treatments that may not be effective or safe, while also helping insurers control expenses and investigate the necessity of specific procedures. Understanding this process is critical for anyone engaging with Kaiser Permanente healthcare services.
Who requires a prior authorization?
Certain services and prescription medications require prior authorization due to their nature, costs, and complexity. Typically, high-cost medications, advanced imaging procedures (like MRIs or CT scans), and specialist referrals fall into this category. The eligibility criteria for these services often vary based on the particular health insurance plan, meaning patients should be proactive in understanding what may require authorization under their specific Kaiser Permanente coverage.
Accessing the Kaiser Permanente Prior Authorization Form
To start the prior authorization process, individuals need to locate the appropriate form. The Kaiser Permanente website provides friendly navigation tools to help users find the right documentation. The online portal is designed to be straightforward, guiding users through each step of the process.
You can find the prior authorization form by logging into the Kaiser Permanente member portal and navigating to the 'Forms' section. Here, users will also find direct links to download the forms as needed. If you experience challenges, you could also seek assistance from customer service to guide you directly to the right resources.
Types of prior authorization forms
There are various prior authorization forms available, each tailored for specific services and medications. Medications may require their unique forms, while surgical procedures and specialist services will have different documentation. Understanding the distinctions is critical for ensuring that the request is processed smoothly. Each form typically includes guidelines that specify which types of requests are appropriate for submission.
Step-by-step instructions for filling out the form
Successfully filling out the prior authorization form involves gathering essential information first. Patients will need to provide their personal details including name, date of birth, and member ID, alongside the provider’s information such as the doctor’s name, contact details, and NPI number. Proper documentation establishes a foundation for the authorization request.
The form itself has several sections that must be accurately completed. The structured arrangement aids clarity in the submission process, while incomplete or incorrect data may lead to delays.
Submitting the Kaiser Permanente prior authorization form
Once the form is completed, the next step is submission. Kaiser Permanente provides multiple avenues for sending the prior authorization form, enabling flexibility based on individual preferences.
Online submission through the patient portal is often the most efficient method. Alternatively, forms can also be submitted via fax or traditional mail, with details often provided within the documentation. Ensure that you retain copies of all submitted forms for your records.
Confirmation of submission
After submission, it's crucial to verify that your prior authorization request has been received. Confirmation may be available online, allowing you to track your request's status. Typically, response timelines vary, so checking back promptly can help alleviate any uncertainties about the request.
Follow-up on your prior authorization request
Monitoring the status of your prior authorization request can be done using various methods. The Kaiser Permanente portal offers a user-friendly interface where members can easily check the status of their request. If you need assistance or updates, reaching out to customer support can provide clarity.
In some cases, additional information may be requested from your provider or you. Rather than delaying the process by neglecting these requests, timely and thorough responses are paramount to expedite the authorization process.
Common issues and troubleshooting
In the event of a denied prior authorization request, understanding the reasons behind the denial is essential. Denials often occur due to incomplete information or failure to adequately demonstrate the medical necessity of the requested service. Engaging with your provider to clarify these details can significantly help.
To appeal a denial, patients typically need to submit a formal appeal letter addressing the reasons for the initial denial. It's important to attach any additional supporting documents that can strengthen your case. Proactively managing this situation is crucial for getting your request reconsidered.
Frequently asked questions
Those new to the Kaiser Permanente prior authorization process often have common questions. For instance, many ask about typical timelines for decisions or what documentation is deemed necessary for a specific request. It’s advisable to refer to the FAQs section on the Kaiser Permanente website or directly ask customer support for personalized assistance.
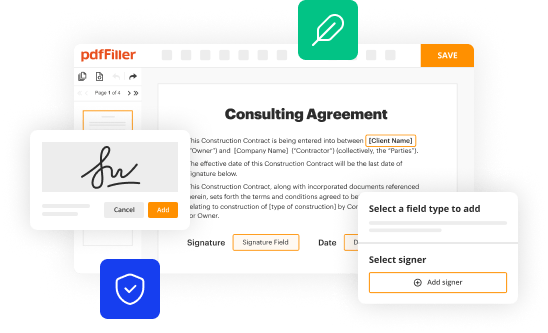
Interactive tools for managing your authorization
pdfFiller’s document management solutions offer valuable features that can help streamline the prior authorization process. Tools for filling, editing, eSigning, and collaborating on documents enhance workflow efficiency, allowing users to tackle forms with ease.
Leveraging these interactive tools can lead to a more organized and efficient approach to handling healthcare paperwork. Utilizing a cloud-based solution ensures that documents are accessible anytime, anywhere, thus simplifying the management of health-related submissions.
Additional insights
The role of prior authorizations in patient care is substantial. While some patients may view this process as a hassle, it serves a greater purpose in promoting cost-effective and necessary treatments. Common misconceptions about prior authorizations include the belief that they delay care unnecessarily, while in reality, they serve as a check to ensure that the recommended treatments are appropriate for the patient's condition.
Looking forward, emerging trends in prior authorization in healthcare include the integration of digital solutions that streamline the submission and approval processes. pdfFiller’s innovation in addressing documentation needs aligns with these advancements, promoting efficiency and patient satisfaction.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my kaiser permanente prior authorization in Gmail?
How do I edit kaiser permanente prior authorization on an Android device?
How do I fill out kaiser permanente prior authorization on an Android device?
What is kaiser permanente prior authorization?
Who is required to file kaiser permanente prior authorization?
How to fill out kaiser permanente prior authorization?
What is the purpose of kaiser permanente prior authorization?
What information must be reported on kaiser permanente prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.