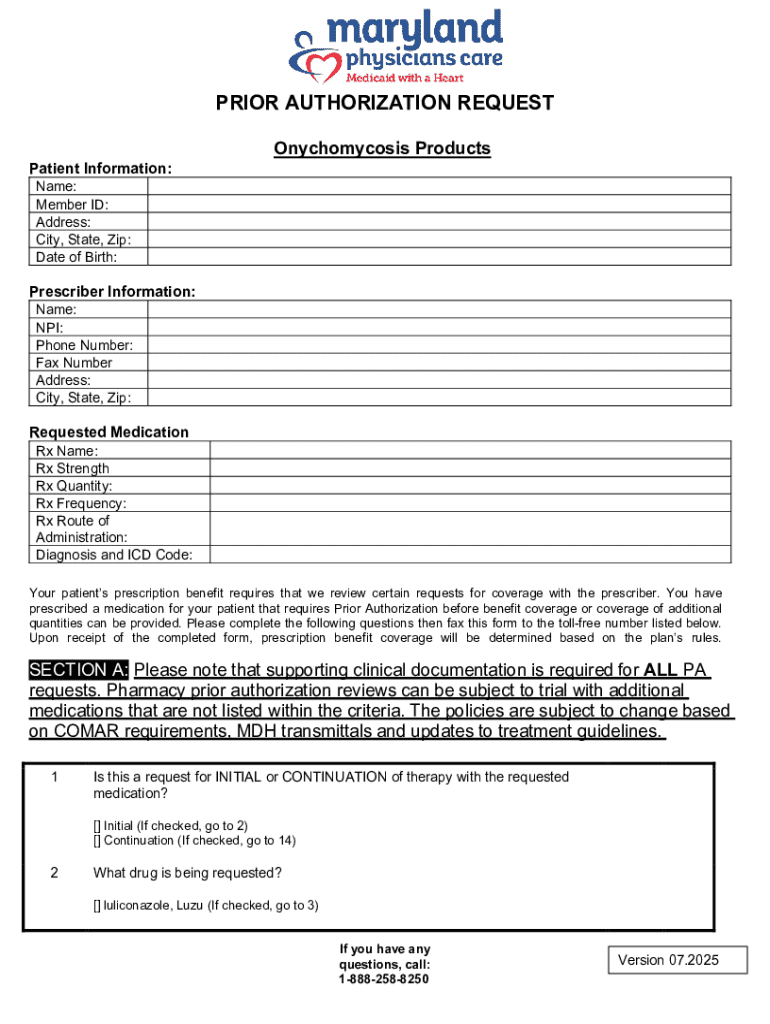
Get the free Prior Authorization Request
Get, Create, Make and Sign prior authorization request



How to edit prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request

How to fill out prior authorization request
Who needs prior authorization request?
A Comprehensive Guide to Prior Authorization Request Forms
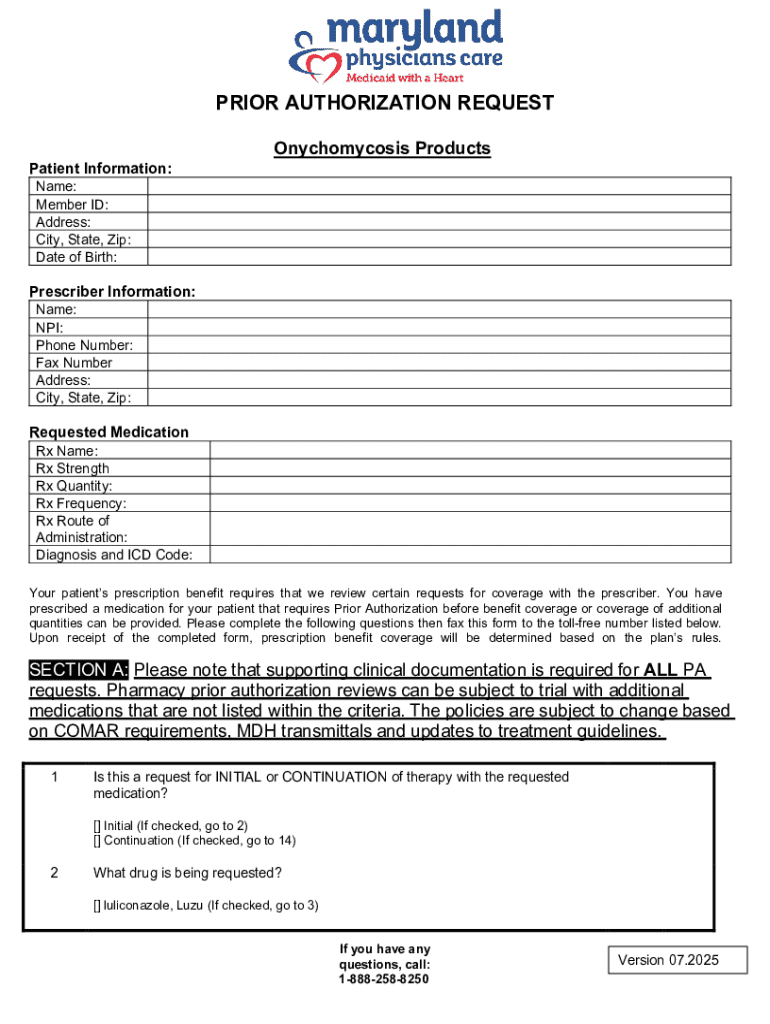
Understanding the prior authorization request form
A prior authorization request form is a critical document in the healthcare process, serving as a formal request from healthcare providers to insurance companies to obtain approval for specific treatments, medications, or services. The purpose of this form is to ascertain that the requested service is medically necessary and falls within the parameters of the patient’s insurance plan. As healthcare costs continue to rise, insurers have increasingly employed prior authorization as a cost-control mechanism.
The importance of prior authorization lies not only in controlling costs but also in ensuring that patients receive appropriate and effective care. This process can help prevent unnecessary procedures and streamline patient management. Common scenarios requiring a prior authorization request include specialized medications, certain diagnostic tests, and advanced imaging services like MRIs or CT scans.
Key components of the prior authorization request form
When filling out a prior authorization request form, several essential components must be included to ensure approval. Accurate and comprehensive data is essential for expediting the authorization process.
Step-by-step guide to completing the prior authorization request form
Completing a prior authorization request form can be a complex task, but following a systematic approach can simplify the process.
Editing and customizing the prior authorization request form
In the digital age, using tools to facilitate the creation and customization of the prior authorization request form can save time and ensure compliance. Utilizing platforms like pdfFiller allows users to easily edit PDFs, eSign, and collaborate on documents within a secure cloud-based environment.
Managing your prior authorization requests
Effective management of prior authorization requests is crucial for ensuring timely patient care. It requires diligence in tracking submissions and understanding the insurer's processes.
Collaborating with your team on prior authorization requests
Collaboration plays a vital role in ensuring that prior authorization requests are filled out accurately and efficiently, especially within multi-disciplinary healthcare settings.
Frequently asked questions (FAQs) about prior authorization requests
Navigating the world of prior authorizations often raises several questions about the process itself. Below are some commonly asked questions.
Further considerations for users of pdfFiller
Using pdfFiller for managing prior authorization requests not only simplifies the editing process but also strengthens data security and compliance efforts, which are critical in healthcare.
Key takeaways
Understanding the intricacies involved in completing a prior authorization request form is essential for healthcare providers and insurance teams alike. By employing best practices throughout the process, from gathering information to submitting forms, users can significantly enhance their chances of approval.
Utilizing tools like pdfFiller enables a more efficient, accurate, and collaborative approach toward managing these documents, ultimately leading to better patient care outcomes. Empowering teams with streamlined document handling ensures that the focus remains where it should be — on patient health and well-being.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find prior authorization request?
How do I make changes in prior authorization request?
How do I fill out prior authorization request on an Android device?
What is prior authorization request?
Who is required to file prior authorization request?
How to fill out prior authorization request?
What is the purpose of prior authorization request?
What information must be reported on prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.