Get the free Vitreomacular Adhesion Prior Authorization Request
Get, Create, Make and Sign vitreomacular adhesion prior authorization
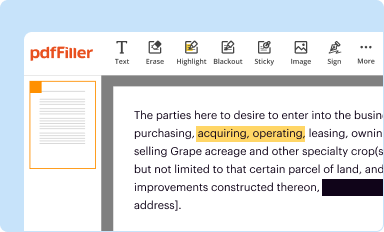
How to edit vitreomacular adhesion prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out vitreomacular adhesion prior authorization
How to fill out vitreomacular adhesion prior authorization
Who needs vitreomacular adhesion prior authorization?
Navigating the Vitreomacular Adhesion Prior Authorization Form
Understanding vitreomacular adhesion
Vitreomacular adhesion (VMA) occurs when the vitreous gel in the eye adheres to the macula, the central part of the retina responsible for detailed vision. This adhesion can lead to various complications, including distortion or loss of central vision, making it essential for both patients and healthcare providers to be familiar with its implications. Effective treatment hinges on early diagnosis, making awareness of the condition critical.
Key symptoms of VMA often include blurred vision, wavy lines when viewing straight edges, and difficulty focusing on text or faces. Risk factors are varied, but age, history of eye surgery, and conditions such as diabetes can heighten the likelihood of developing VMA. Understanding these symptoms and risk factors is vital for timely intervention, which may involve therapies aimed at relieving the adhesion and restoring vision.
Prior authorization: What you need to know
Prior authorization refers to the process where healthcare providers must obtain approval from a patient's insurance company before a specific treatment is covered. This step ensures that the proposed treatment aligns with the patient's medical necessity according to the insurance guidelines. In the context of VMA, prior authorization is often critical for therapies that can alleviate symptoms and prevent serious vision loss.
Many patients harbor misconceptions about the prior authorization process, viewing it as an unnecessary hurdle. However, it serves as a safeguard to validate treatment plans, ensuring they are clinically justified. Understanding how this process works can empower patients to advocate for their healthcare needs effectively.
Overview of the vitreomacular adhesion prior authorization form
The vitreomacular adhesion prior authorization form is a crucial document that outlines the necessity of treatment for patients diagnosed with VMA. Typically, healthcare providers submit this form to insurance companies before commencing treatment options such as injections or surgical procedures. The completion and approval of this form facilitate the efficient processing of claims, ensuring that patients receive earlier access to necessary care.
Usually, this form is required by the healthcare provider after an initial diagnosis of VMA, particularly when the proposed intervention exceeds standard practice guidelines. The key sections of this form include patient demographics, medical history, details about previous treatments, and necessary supporting documents that substantiate the need for the proposed treatment.
Step-by-step guide to filling out the VMA prior authorization form
Gathering necessary information
Before beginning the VMA prior authorization form, gathering comprehensive documentation is crucial. Begin by collecting the patient’s complete medical history, including any previous diagnoses, treatments, and imaging results that pertain to VMA. Complete and accurate patient information, including insurance details and contact information, is essential for a smooth submission process.
Completing the form
As you fill out the form, ensure that each section is completed meticulously. Start with the patient demographics, listing clear details such as the patient's name, date of birth, and insurance information. In the medical history section, detail previous diagnoses related to VMA and include any symptoms experienced. This should be followed by a detailed account of any prior treatments and their outcomes along with accompanying medical documentation, such as imaging reports, to reinforce the treatment necessity.
Reviewing your submission
Once the form is completed, reviewing it for accuracy and completeness is vital. Double-check all sections, ensuring that no information has been omitted. Common errors often include missing patient identifiers, incomplete medical histories, or inadequate support for the requested treatment. Identifying and resolving these errors can greatly enhance the approval chances.
Techniques for efficient form submission
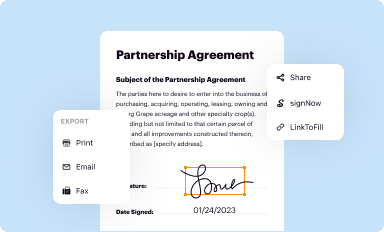
Minimizing processing delays during submission can significantly streamline patient care. One effective approach is to ensure that all required documentation is organized and submitted concurrently with the prior authorization form. Additionally, utilizing electronic submission options can hasten processing times, as many insurance companies offer online platforms that are quicker compared to traditional mail.
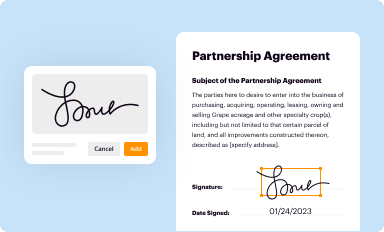
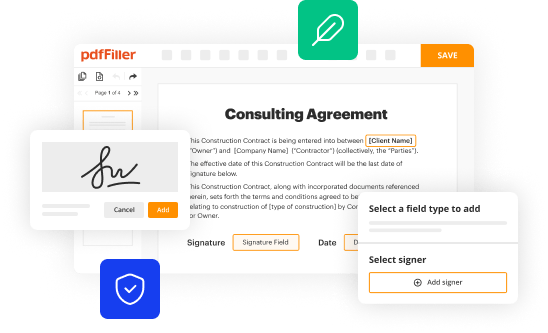
Using tools like pdfFiller allows for digital signing and effortless editing, facilitating a more efficient submission process. Enhance workflow with features that enable easy merging of documents, ensuring everything is in one place. Such strategies minimize the risk of delays, allowing patients to receive timely treatment.
Follow-up: What happens next after submission?
Following the submission of the VMA prior authorization form, insurance companies will initiate their review process. This typically involves assessing the form and its accompanying documents to determine the medical necessity for the proposed treatment. The approval or denial timeline varies by insurer, but most aim to provide a decision within a few days to a couple of weeks.
If the authorization request is denied, it's crucial to take immediate action. Understanding the reasons for the denial can guide the steps for resubmission or appeal. Patients should consult with their healthcare provider to discuss alternative treatment routes or additional documentation that may strengthen the case for approval.
Tips for appeals and resubmission
When faced with a denial of your prior authorization request, understanding the appeals process is essential. Reach out to the insurance company to clarify the specific reasons for the denial. In your appeal, clearly articulate why the treatment is medically necessary, and include any updated documentation that may support this claim. Thoroughness in your response can significantly impact the appeals outcome.
Persistence is vital in the appeals process. Do not hesitate to follow up regularly with the insurance provider until resolution is achieved. A well-documented appeal that addresses all points of contention from the denial will bolster your chances of obtaining the necessary authorization.
Utilizing pdfFiller for your documentation needs
Employing pdfFiller for completing the VMA prior authorization form offers several advantages. This platform allows users to seamlessly edit PDFs, eSign documents, and collaborate effectively, enabling smooth communication between healthcare providers and patients. The range of features available through pdfFiller, such as template creation and real-time collaboration tools, enhances the documentation process.
Moreover, the platform provides secure storage for submitted forms, allowing users to easily manage their documentation needs. This not only enhances accessibility but also ensures patient data is kept confidential and organized.
Frequently asked questions (FAQs)
Many individuals have common queries regarding the vitreomacular adhesion prior authorization form. Questions often revolve around what constitutes necessary information, how long the insurance review process takes, and the implications of denial. Understanding the answers to these queries can demystify the process and reduce anxiety associated with navigating insurance protocols.
Patients may also have concerns about how the prior authorization can affect their treatment timeline. Having clear responses to these frequently asked questions lays the groundwork for informed patient engagement and proactive healthcare management.
Contact information for further assistance
For those needing additional support with the vitreomacular adhesion prior authorization form, reaching out to help teams affiliated with your insurance provider can be invaluable. These teams are equipped to guide patients through the authorization process, clarifying any confusion about required documentation or the review timeline.
Moreover, consulting with your healthcare provider throughout this process ensures that you are making informed decisions regarding your treatment and insurance needs. Building a collaborative relationship between patients and providers can greatly enhance the efficiency of the authorization process.
Support resources
Links to relevant medical resources or organizations specializing in vitreomacular adhesion can serve as valuable reference points for both patients and providers. Additionally, pdfFiller is not only beneficial for VMA forms but also offers extensive document-related solutions for various needs, empowering users to manage their healthcare documentation efficiently.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete vitreomacular adhesion prior authorization online?
How do I complete vitreomacular adhesion prior authorization on an iOS device?
How do I edit vitreomacular adhesion prior authorization on an Android device?
What is vitreomacular adhesion prior authorization?
Who is required to file vitreomacular adhesion prior authorization?
How to fill out vitreomacular adhesion prior authorization?
What is the purpose of vitreomacular adhesion prior authorization?
What information must be reported on vitreomacular adhesion prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.