Get the free Proton Pump Inhibitors Preauthorization
Get, Create, Make and Sign proton pump inhibitors preauthorization



Editing proton pump inhibitors preauthorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out proton pump inhibitors preauthorization

How to fill out proton pump inhibitors preauthorization
Who needs proton pump inhibitors preauthorization?
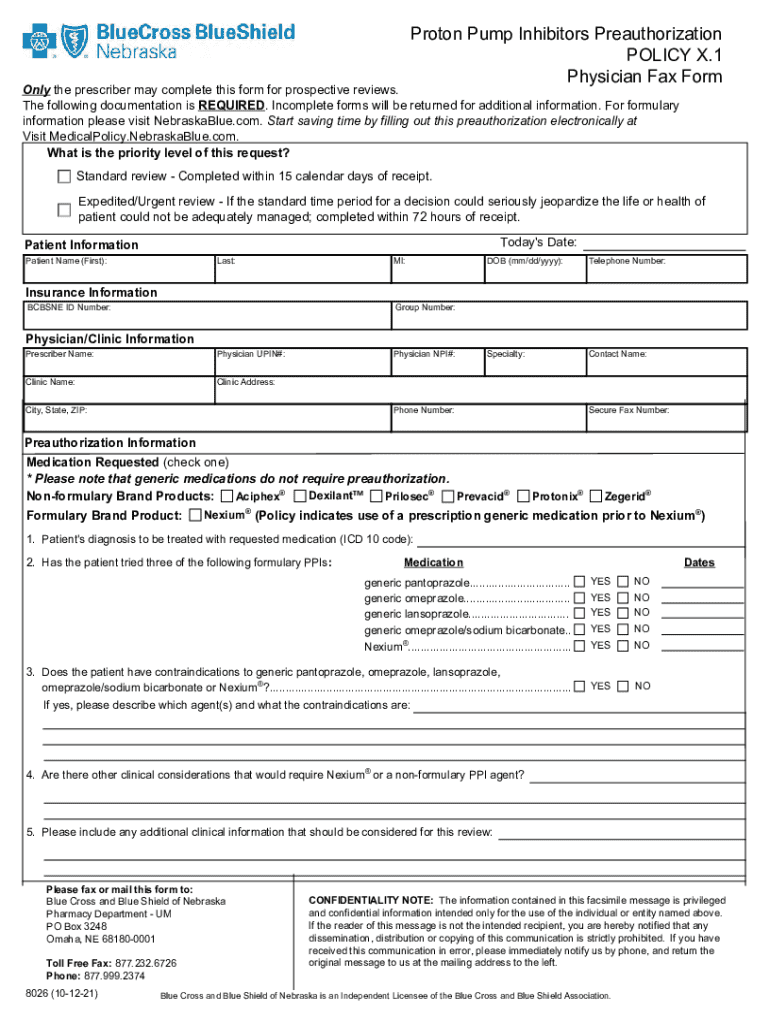
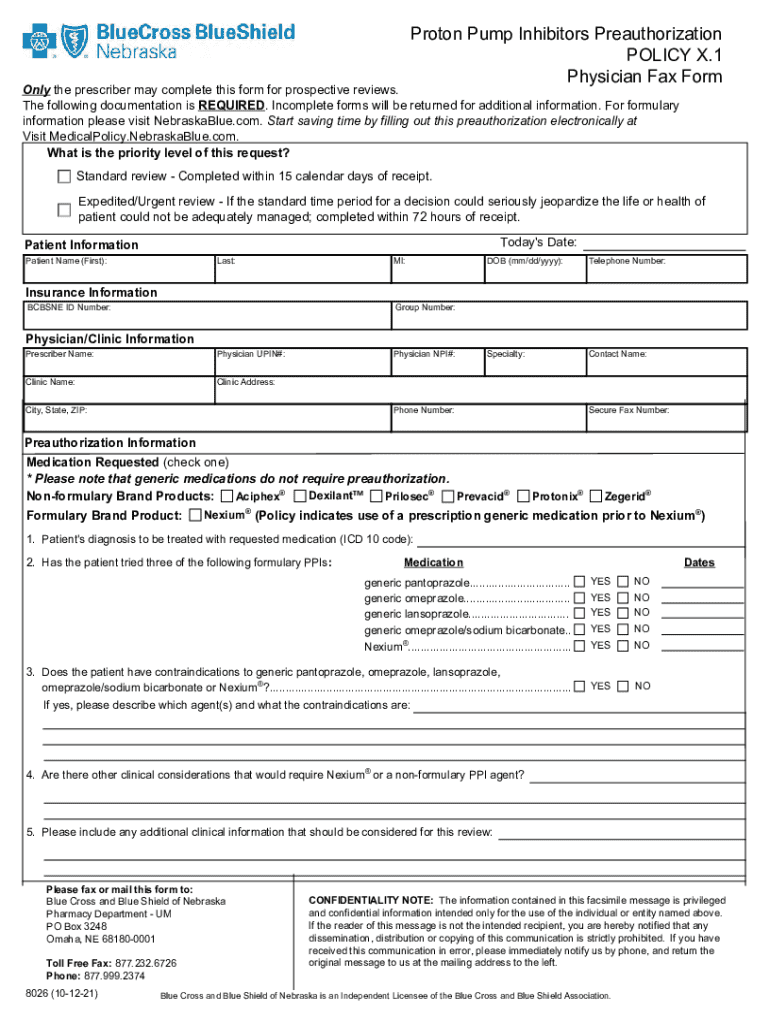
Understanding the Proton Pump Inhibitors Preauthorization Form
Understanding proton pump inhibitors (PPIs)
Proton pump inhibitors (PPIs) are a class of medications that reduce stomach acid production. They are primarily used to treat conditions such as gastroesophageal reflux disease (GERD), peptic ulcers, and Zollinger-Ellison syndrome. By blocking the proton pump in the stomach lining, these medications help alleviate symptoms and promote healing of the gastrointestinal tract. Given their widespread use, understanding the importance of proper preauthorization for PPI coverage is crucial.
Preauthorization is the process required by health insurers before certain medications, like PPIs, are covered. This requirement ensures that allergic reactions, contraindications, or alternative treatments have been considered before a costly medication is dispensed. As PPIs can have significant interactions and side effects, securing preauthorization helps manage both patient safety and costs.
What is a preauthorization form?
A preauthorization form is a document submitted to an insurance provider, requesting approval for coverage of a specific medication or treatment before it is administered. This process is essential in controlling healthcare costs and ensuring that patients receive appropriate care based on their medical history and diagnosis.
For PPIs, preauthorization is particularly significant due to their potential impact on health if misused. Insurance companies require this form to confirm eligibility for coverage based on specific criteria, such as medical necessity, previous treatment failures, and condition-based guidelines.
Components of the PPI preauthorization form
To successfully submit a preauthorization request for PPIs, understanding the various components of the form is essential. The form typically consists of several sections, each crucial for processing the request efficiently.
In addition to the filled-out sections, the form may require supporting medical records and a summary outlining previous treatments. These documents provide context and rationale for the request, helping insurers make informed decisions.
Step-by-step guide to completing the PPI preauthorization form
Filling out the PPI preauthorization form requires attention to detail and accurate information. Here's a step-by-step guide to streamline the process.
Submitting the PPI preauthorization form
Once the preauthorization form is completed, the next step is submission. Depending on the healthcare provider’s preference, there are different methods available to submit the PPI preauthorization form.
After submitting the request, it’s essential to monitor the status. Insurers typically provide expected response timeframes, usually ranging from a few days to a few weeks.
Managing challenges and denials
Despite thorough preparations, preauthorization requests for PPIs can sometimes be denied. Understanding common reasons for denial can help healthcare providers and patients strategize effectively.
If a preauthorization request is denied, the first step is to review the denial letter carefully. A clear outline of the appeal process will be provided, which typically includes submitting additional information or clarification.
Communication with healthcare providers is crucial during this process. Engaging them in writing an effective appeal can significantly improve the chances of approval.
Interactive tools for managing your preauthorization needs
Utilizing interactive tools can simplify the preauthorization process substantially. pdfFiller offers various features tailored for this need.
To use pdfFiller for filling out the PPI form, users should access the platform and follow straightforward step-by-step instructions, enhancing efficiency and reducing errors.
Best practices for efficient preauthorization management
To ensure a smooth preauthorization process for PPIs, best practices should be followed diligently.
Frequently asked questions (FAQs)
Various concerns arise regarding the PPI preauthorization process. Addressing common questions can clear up confusion and assist in managing expectations.
Conclusion on the benefits of using a preauthorization form for PPIs
The PPI preauthorization form is not merely a bureaucratic hurdle; it serves as a safeguard for both patients and insurers, ensuring that treatment plans are medically necessary and economically feasible. Using this form properly streamlines access to treatment while protecting financial interests.
Adopting best practices, leveraging innovative tools like those offered by pdfFiller, and maintaining clear communication between healthcare providers and insurers will enhance the efficiency of the preauthorization process. This ultimately leads to better patient outcomes and effective management of healthcare resources.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my proton pump inhibitors preauthorization directly from Gmail?
How do I fill out proton pump inhibitors preauthorization using my mobile device?
Can I edit proton pump inhibitors preauthorization on an Android device?
What is proton pump inhibitors preauthorization?
Who is required to file proton pump inhibitors preauthorization?
How to fill out proton pump inhibitors preauthorization?
What is the purpose of proton pump inhibitors preauthorization?
What information must be reported on proton pump inhibitors preauthorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.