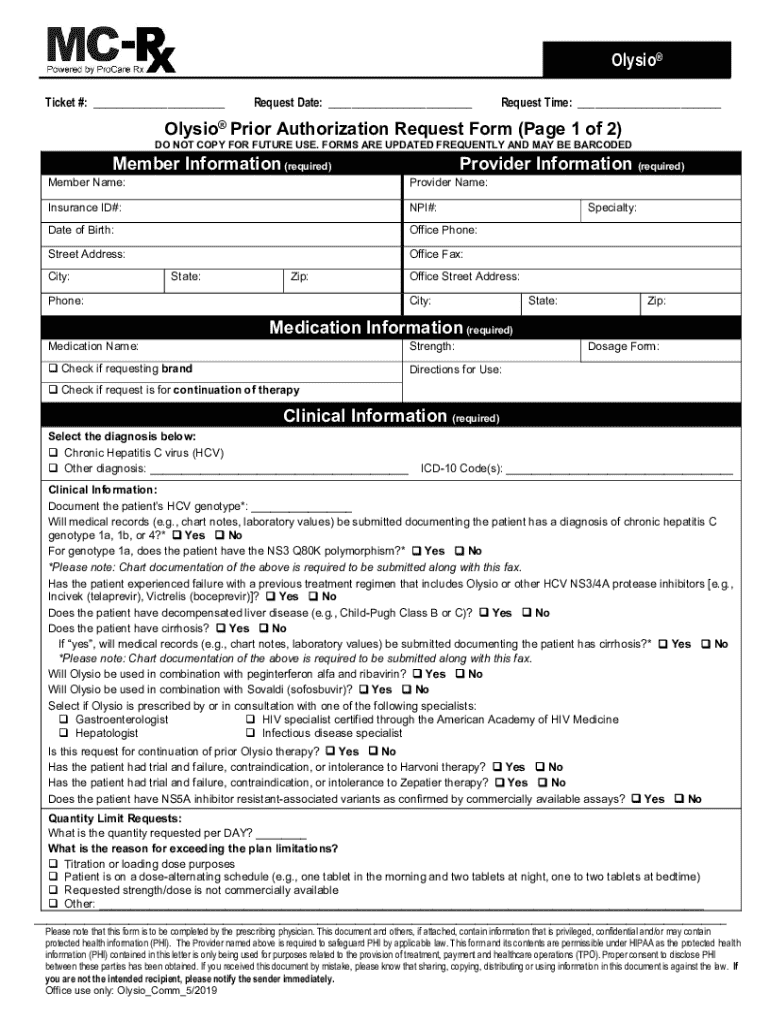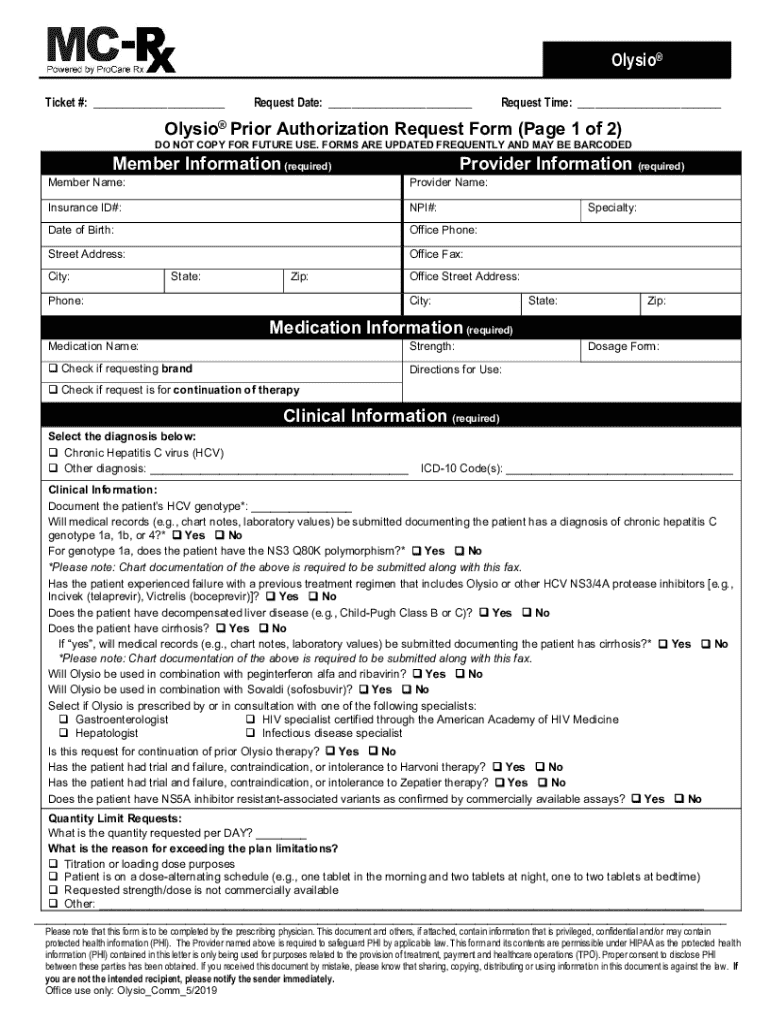
Get the free Olysio® Prior Authorization Request Form
Get, Create, Make and Sign olysio prior authorization request
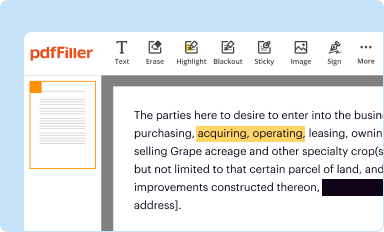
Editing olysio prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out olysio prior authorization request
How to fill out olysio prior authorization request
Who needs olysio prior authorization request?
Comprehensive Guide to the Olysio Prior Authorization Request Form
Understanding Olysio and its necessity
Olysio, generically known as simeprevir, is an antiviral medication approved for the treatment of chronic hepatitis C. This medication operates by inhibiting the virus's ability to replicate, which is crucial for managing this serious disease. It is often indicated for patients with specific genotypes of hepatitis C, primarily genotype 1, and is frequently used in combination with other treatments, such as sofosbuvir. Understanding its implications is essential as the patient demographics vary, but the need for effective management remains consistent across the board.
Prior authorization plays a critical role in the prescribing process. This is a cost-control measure that ensures the medication is necessary and that the patient meets certain criteria before the insurance provider will cover the medication. For Olysio, prior authorization is especially vital due to the medication's considerable expense and the need to confirm its appropriate use according to treatment guidelines.
Overview of the Olysio prior authorization request form
The Olysio prior authorization request form is a prerequisite for healthcare providers seeking to prescribe this medication for patients. This form is designed to streamline the approval process for insurance companies, ensuring they have the necessary information to make informed decisions about coverage. The primary aim of the form is to document the patient’s medical necessity for Olysio, providing evidence of prior treatments and health conditions that necessitate its use.
Both patients and healthcare providers must be involved in completing this form. Patients provide personal information while providers fill out detailed medical data. Insurance companies review this documentation to confirm eligibility, making it crucial for effective communication among all parties involved.
Key sections of the Olysio prior authorization request form
Each section of the Olysio prior authorization request form serves a purpose to facilitate the review process by insurance providers. Below are the key components to be filled in:
Step-by-step instructions for completing the form
Completing the Olysio prior authorization request form can be straightforward if you follow a systematic approach. The following steps outline how to efficiently fill out the form.
It’s crucial to avoid common pitfalls, such as omitting required fields or providing incomplete information, as these errors can significantly delay the approval process.
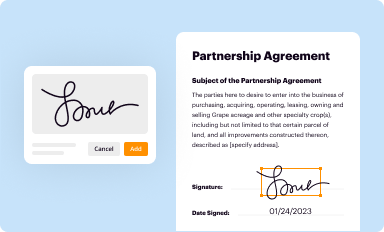
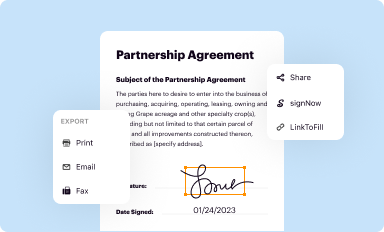
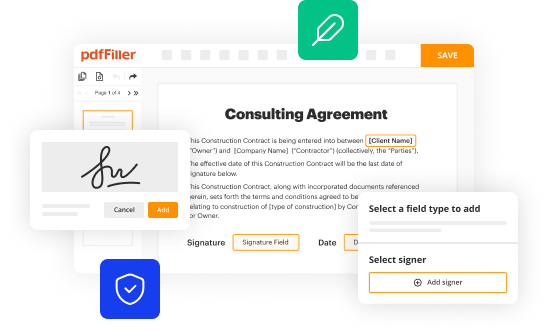
Interactive tools for form management
Managing the Olysio prior authorization request form can be enhanced through the use of tools such as pdfFiller. This cloud-based service specializes in helping users create, edit, and manage forms conveniently.
These interactive tools not only streamline the process but also enable users to manage documentation from anywhere, ensuring easy access and collaboration.
Submitting the Olysio prior authorization request
Once the Olysio prior authorization request form is complete, the next step involves submission. Preparation is key to ensure that all necessary information is included, which can facilitate a smoother review process.
Selecting the appropriate channel can depend on insurer preferences or the urgency of the request.
Tracking the status of your authorization request
After submission of the Olysio prior authorization request, it’s important to monitor its progress. Different methods exist for tracking authorization status and communicating with insurance providers.
Understanding these outcomes can help in managing next steps effectively.
Next steps if your authorization is denied
Receiving a denial for the Olysio prior authorization request can be disheartening, but it’s essential to analyze the reasons given. Common denial reasons may include a lack of medical necessity or insufficient documentation.
Navigating denials can be complex, but being proactive in understanding and addressing the reasons can facilitate the approval process.
Tips for a successful Olysio authorization experience
Achieving success with the Olysio prior authorization request does not solely rely on filling out forms; it involves a holistic approach from both healthcare providers and patients.
Implementing these strategies helps create a more efficient authorization experience, ultimately benefiting patient care.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find olysio prior authorization request?
How do I edit olysio prior authorization request on an iOS device?
Can I edit olysio prior authorization request on an Android device?
What is olysio prior authorization request?
Who is required to file olysio prior authorization request?
How to fill out olysio prior authorization request?
What is the purpose of olysio prior authorization request?
What information must be reported on olysio prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.