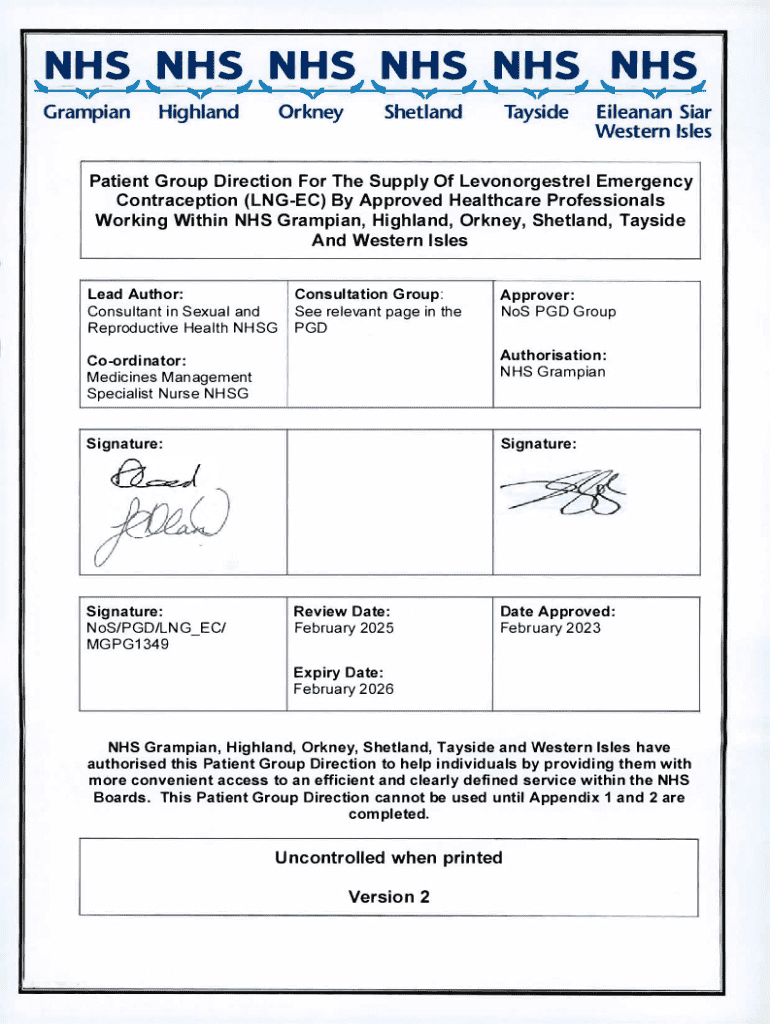
Get the free Patient Group Direction for the Supply of Emergency Contraception
Get, Create, Make and Sign patient group direction for



Editing patient group direction for online
Uncompromising security for your PDF editing and eSignature needs
How to fill out patient group direction for

How to fill out patient group direction for
Who needs patient group direction for?
Patient group direction for form - How-to guide
Understanding patient group directions (PGDs)
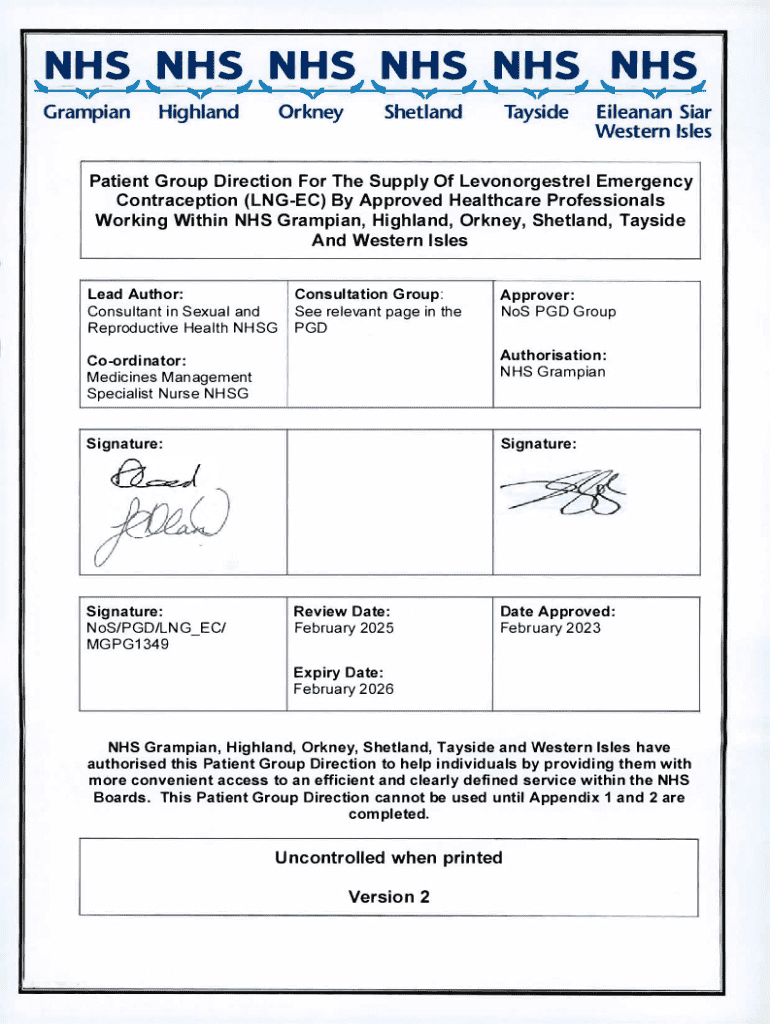
Patient Group Directions (PGDs) are specific frameworks that authorize named health professionals to supply and administer specific medicines to groups of patients without the need for a prescription. Their primary purpose is to streamline healthcare services, improving access to medications for patient groups that typically face barriers to timely treatment.
The importance of PGDs transcends mere convenience; they enhance the efficiency of healthcare delivery, especially in settings such as clinics, community health services, and during public health initiatives. By allowing trained practitioners to administer medications directly, PGDs can reduce waiting times and foster patient satisfaction.
Legally, PGDs are governed by the Human Medicines Regulations 2012 in the UK and similar regulations worldwide, which require a thorough understanding of both the clinical implications and the legal responsibilities involved in their use.
Key components of a patient group direction
An effective PGD is documented carefully and should contain several essential components. First, it must include a clear description of the medicines involved—details such as dosage, route of administration, associated side effects, and contraindications are critical for safe practice.
Identifying the authorized health practitioners is another vital component. The document should explicitly state which qualified professionals can operate under the PGD and their specific roles. Finally, thorough documentation and record-keeping practices are essential; this includes maintaining patient records, audits, and compliance checks to ensure continuous adherence to the PGD.
The process of developing a PGD
Creating a PGD is a multi-step process that begins with assessing the need for such a directive. This involves identifying patient groups requiring specific treatments and evaluating the clinical needs based on the healthcare services provided in the region.
Once the need is established, planning and preparation can commence. Engaging stakeholders—including healthcare professionals and patient representatives—is crucial, as it ensures the PGD meets the targeted community's needs and outlines clear objectives and expected patient outcomes.
The actual writing of the PGD involves drafting a template that is both comprehensive and user-friendly. Clarity in language and terminology is paramount; anyone referencing or using the PGD should easily understand its instructions and implications.
Following the draft, the PGD enters an authorization phase where it requires review and sign-off by the designated legal educators. This phase ensures that all legal and ethical considerations are thoroughly addressed.
Implementing the PGD in practice
Once developed and approved, the next critical step is training the healthcare practitioners who will be utilizing the PGD. Developing comprehensive training programs will equip practitioners with the knowledge needed to operate effectively within the guidelines of the PGD. Continuous Professional Development (CPD) opportunities can help maintain relevant skills and updates on the latest practices.
After training, integrating PGDs into practice workflow is essential for effective implementation. This might involve specific documentation protocols that healthcare workers can follow when interacting with patients under the guidance of the PGD. It ensures consistency and safety throughout clinical settings.
Monitoring and reviewing PGDs
Evaluating the effectiveness of a PGD post-implementation is vital. Performance indicators and measurement tools can be utilized to gauge its success. Gathering feedback from healthcare practitioners who implement the PGD is equally important, as they can provide insights into any challenges or areas for improvement.
When updates are necessary, knowing how and when to revise existing PGDs is essential. As medicines, guidelines, and patient needs evolve, keeping PGDs current and relevant is key to continued success in your healthcare setting.
Navigating common challenges with PGDs
Implementing PGDs can sometimes encounter barriers—common challenges include legal uncertainties and resistance from practitioners unfamiliar with PGD processes. Identifying these obstacles early can facilitate more considerable support for effective PGD strategies.
Solutions might involve further training, clarifying legal guidelines, and sharing case studies of successful PGD implementations to encourage acceptance and understanding amongst staff. Lessons learned from past implementations can guide organizations toward smoother future experiences.
Additional considerations for effective PGD management
Utilizing technology can significantly enhance PGD document management. Platforms like pdfFiller offer tools for creating and editing PGDs efficiently, fostering collaboration among healthcare teams. Features like eSigning and cloud-based document management allow for swift ordering and administration of medications through PGDs.
Moreover, incorporating PGDs into public health initiatives can augment disease management efforts, significantly improving health outcomes for large populations. Encouraging interdisciplinary collaboration can lead to more robust PGD frameworks and innovative approaches to patient care.
Best practices for maintaining compliance
Maintaining compliance with PGDs requires diligent adherence to legal and regulatory standards. Establishing periodic review and audit procedures ensures that practice standards are continuously met. Leveraging professional networks allows for support, resource sharing, and knowledge exchange among practitioners navigating similar challenges.
Regularly reviewing PGD documents not only ensures their relevance but also supports best practices in patient care.
Resources and tools for PGD development
To assist in the development of PGDs, numerous resources and tools can enhance the process. Templates designed for PGDs can streamline initial drafts and ensure that all necessary components are included. Additionally, linking to regulations and best-practice guidance can inform users about legal obligations and standards.
Professional training programs and continuing education opportunities serve as invaluable resources for healthcare practitioners aiming to deepen their understanding of PGD application and relevance in their practice.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my patient group direction for directly from Gmail?
How can I edit patient group direction for from Google Drive?
How do I complete patient group direction for on an iOS device?
What is patient group direction for?
Who is required to file patient group direction for?
How to fill out patient group direction for?
What is the purpose of patient group direction for?
What information must be reported on patient group direction for?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.