Get the free Rybrevant (amivantamab-vmjw) Prior Authorization Form
Get, Create, Make and Sign rybrevant amivantamab-vmjw prior authorization



How to edit rybrevant amivantamab-vmjw prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out rybrevant amivantamab-vmjw prior authorization

How to fill out rybrevant amivantamab-vmjw prior authorization
Who needs rybrevant amivantamab-vmjw prior authorization?
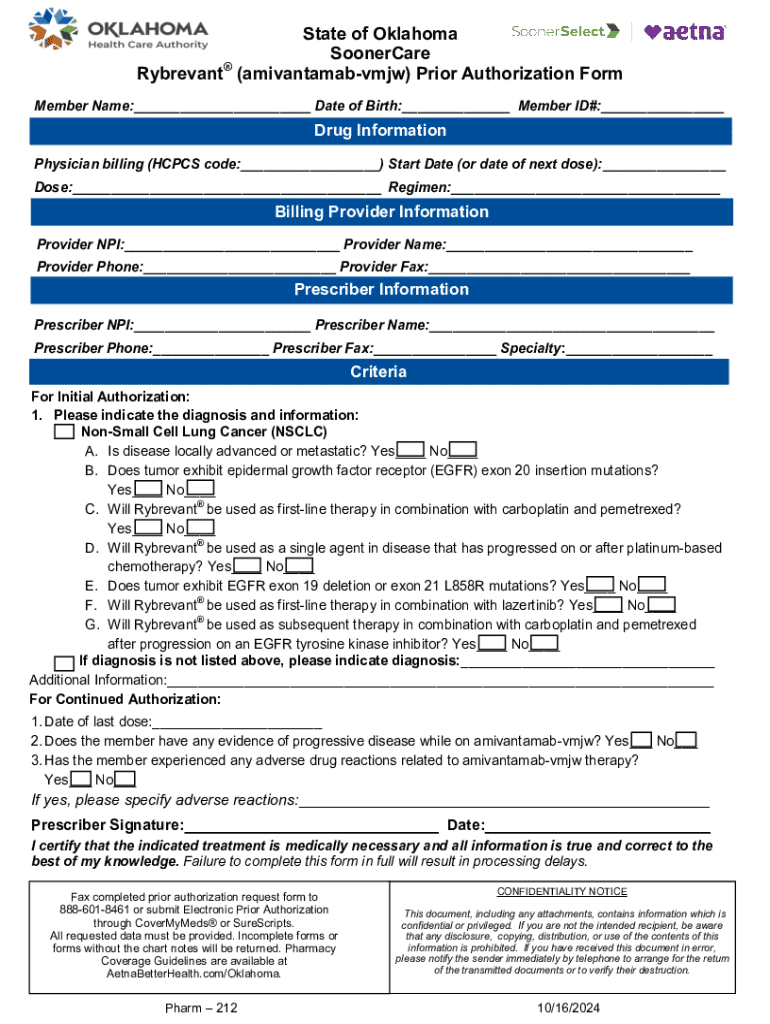
Navigating the Rybrevant (Amivantamab-vmjw) Prior Authorization Form
Overview of Rybrevant (Amivantamab-vmjw)
Rybrevant, known by its generic name Amivantamab-vmjw, is a monoclonal antibody designed to target and inhibit the activity of EGFR (epidermal growth factor receptor) and MET (mesenchymal-epithelial transition factor) proteins. It is primarily indicated for the treatment of patients with non-small cell lung cancer (NSCLC) whose tumors exhibit specific genetic alterations. This innovative therapy is particularly significant for patients with epidermal growth factor receptor (EGFR) exon 20 insertion mutations, providing a much-needed treatment option in a complex healthcare landscape.
The importance of prior authorization in healthcare cannot be overstated. Prior authorization is a managed care process that requires healthcare providers to obtain permission from a patient's insurance company before administering a specific treatment. This practice serves several functions, including ensuring that the prescribed treatment is medically necessary, evaluating cost-effectiveness, and complying with treatment guidelines. For Rybrevant, obtaining prior authorization is essential as it allows insurers to validate the necessity of the treatment based on a patient’s specific medical condition and treatment history.
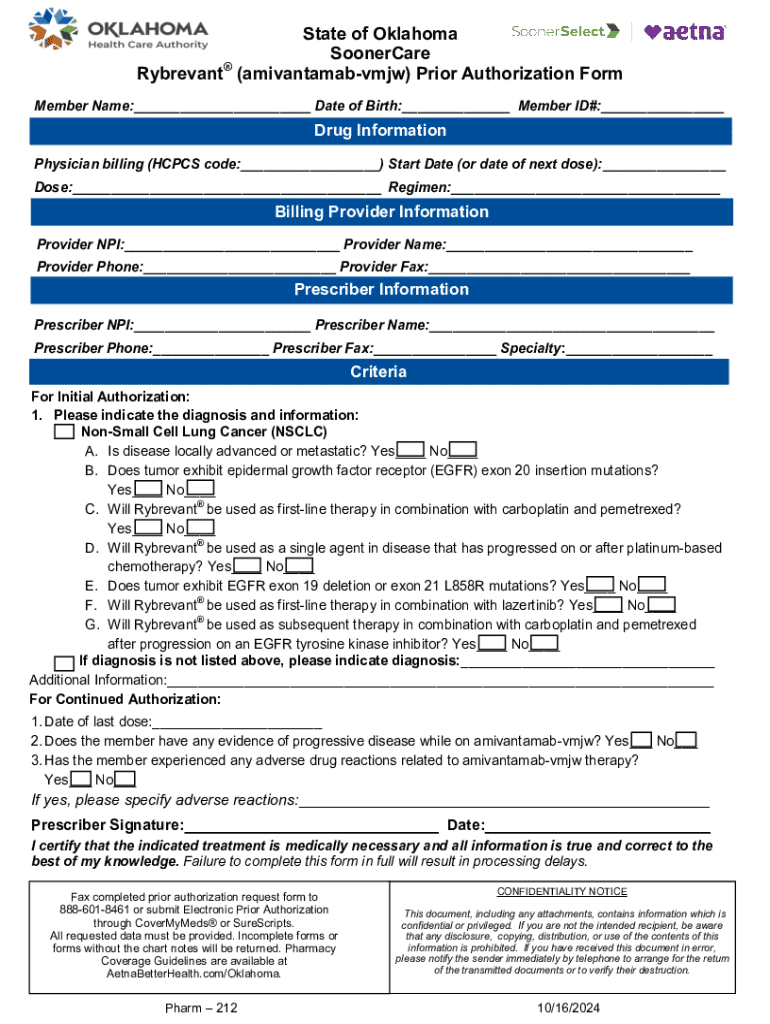
Key elements of the prior authorization form
When it comes to the Rybrevant (Amivantamab-vmjw) prior authorization form, certain key information must be completed for successful submission. First and foremost, essential patient demographics are required, including the patient's name, address, date of birth, and insurance policy number. Additionally, relevant insurance information such as policy details and contact numbers is critical to ensure smooth processing of the authorization request.
Healthcare provider details play an equally important role in the form. This includes the prescribing physician’s name, credentials, contact information, and the practice address. Moreover, drug-specific information must be meticulously filled out, such as dosage and administration details, previous therapies administered, and any relevant laboratory results that substantiate the medical necessity of Rybrevant for the patient in question.
Step-by-step guide to completing the prior authorization form
Completing the prior authorization form can feel like a challenging task. Starting with a preliminary assessment, it’s crucial to verify the specific insurance requirements for Rybrevant as each insurance company may have differing criteria. Confirming the patient's eligibility criteria is also essential — ensure that they have the appropriate diagnosis and have not exceeded the medical necessity thresholds set by their insurance provider.
When filling out the form, break it down section by section. Begin with the Patient Information section, capturing all required demographics accurately. Next, provide Prescribing Physician Details, including all necessary credentials. The Medical Necessity Justification section is vital; clearly state why Rybrevant is necessary for the patient's treatment plan, referencing any relevant clinical guidelines or previous treatment failures. To enhance your submission, be mindful of common mistakes. Overlooking required signatures or providing incomplete patient history can lead to unnecessary delays or even denials.
Submission process for the authorization form
Once the form is completed, reviewing and performing final checks is paramount. Ensure all requisite documents, such as the patient's medical history and authorization signature, are attached. double-check the completeness and accuracy before submission, as minimal errors can complicate the approval process. Various submission methods exist, with electronic submission typically being the most efficient. Familiarize yourself with the specific processes of the insurance provider, which may vary widely in their requirements whether using fax, mail, or an online portal.
Timing expectations are another important factor to consider. Typical review times by insurers can range from a few days to several weeks, depending on the complexity of the case and the insurer’s protocols. After submitting the form, set reminders to follow up regarding the status of the authorization request, ensuring that you stay proactive in case additional information is required.
What to do after submission
Upon submission of the Rybrevant prior authorization form, it’s crucial to prepare for potential denials or requests for additional information. If authorization is denied, promptly review the reason for denial and address any discrepancies. Resubmitting an appeal may require additional modules or testimonials from the prescribing physician to support the necessity for Rybrevant. Navigating this process can be daunting, but maintaining open communication with the insurance provider is essential for resubmission success.
Tracking the status of your authorization request should be a priority right after submission. Most insurance companies provide portals or customer service numbers through which you can check the status of your submission. Utilize these tools to ensure that you are informed promptly if anything was missing or if further information needs to be provided.
Leveraging pdfFiller for efficient form management
Using pdfFiller can greatly enhance your experience with completing and managing the Rybrevant prior authorization form. The platform allows you to edit forms seamlessly, including customizing fields specific to the patient's needs, such as dosage adjustments or additional notes. Templates for the prior authorization request can be saved and reused, streamlining the process for future requests.
Collaboration within healthcare teams is also simplified through pdfFiller. The ability to share forms securely with colleagues or specialists facilitates quicker reviews and real-time feedback on necessary modifications. Additionally, eSigning the authorization form is easy; using digital signatures complies with legal requirements, thus ensuring that the authorization request is valid and adheres to healthcare regulations.
Additional considerations
For patients requiring Rybrevant, various patient assistance programs may be available to alleviate the financial burden associated with treatment. Pharmaceutical companies often have initiatives designed to help patients access medications, particularly for those who may struggle with co-pays or insurance limitations. It is advisable for healthcare providers to keep abreast of evolving patient support resources and programs.
Frequently asked questions about the prior authorization process for Rybrevant center around eligibility, typical timelines for review, and common reasons for denials. Ensuring clarity and preparedness in addressing these inquiries can help mitigate patient anxiety about their treatment options. Engaging with the insurer for precise guidance will provide better insights into the expectations surrounding the prior authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my rybrevant amivantamab-vmjw prior authorization in Gmail?
How can I get rybrevant amivantamab-vmjw prior authorization?
How do I complete rybrevant amivantamab-vmjw prior authorization online?
What is rybrevant amivantamab-vmjw prior authorization?
Who is required to file rybrevant amivantamab-vmjw prior authorization?
How to fill out rybrevant amivantamab-vmjw prior authorization?
What is the purpose of rybrevant amivantamab-vmjw prior authorization?
What information must be reported on rybrevant amivantamab-vmjw prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.