Get the free Nayzilam Prior Approval Request
Get, Create, Make and Sign nayzilam prior approval request



Editing nayzilam prior approval request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nayzilam prior approval request

How to fill out nayzilam prior approval request
Who needs nayzilam prior approval request?
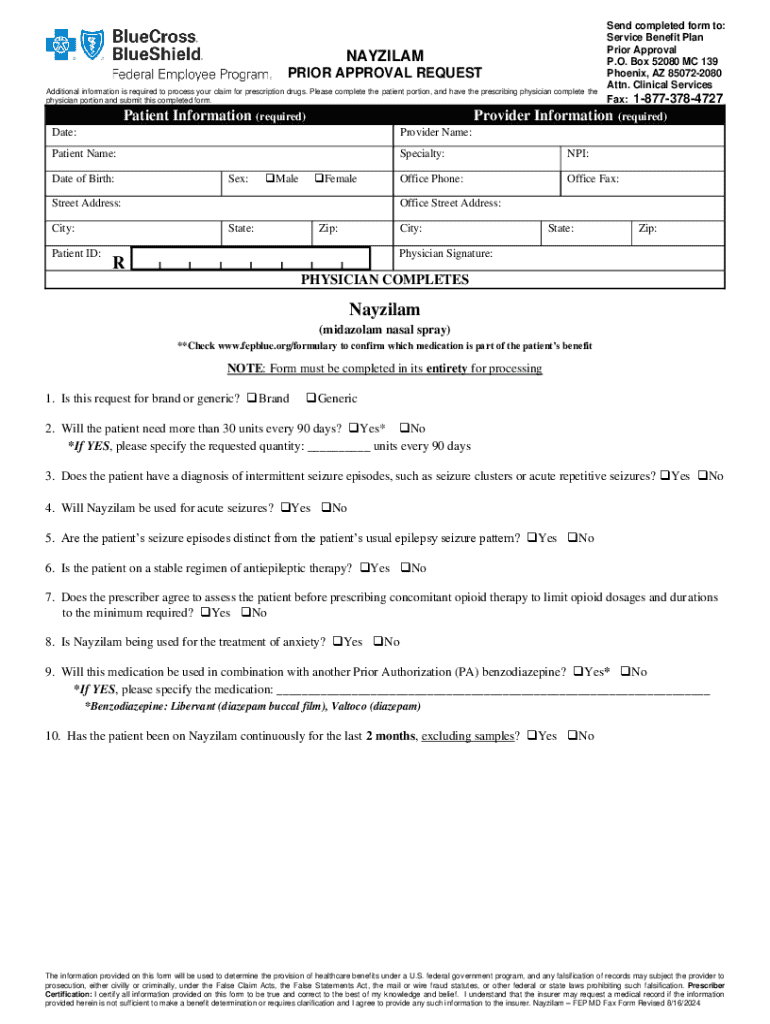
Understanding the Nayzilam Prior Approval Request Form
Understanding Nayzilam: Overview of the Medication
Nayzilam, generically known as midazolam nasal spray, is an important medication primarily designed for treating seizure clusters in individuals with epilepsy. Approved by the FDA in 2019, it provides a rapid response to patients experiencing seizures, allowing for timely intervention that can prevent further complications. Its ease of use is particularly significant for patients in emergency situations where oral medications may not be effective or feasible.
The significance of Nayzilam extends beyond just its immediate pharmacological effects; it addresses a critical need among the over 3.4 million people living with epilepsy in the United States alone. According to the Epilepsy Foundation, nearly 30% of these individuals struggle with treatment-resistant forms, making medications like Nayzilam essential for improving their quality of life and safety.
Importance of prior approval in healthcare
Prior approval, also known as prior authorization, is a crucial process in healthcare that requires healthcare providers to obtain approval from a patient's insurance company before administering specific medications. This process ensures that the prescribed treatment is necessary and complies with the insurance policy's guidelines. While it may seem cumbersome, prior approval serves to protect patients and providers by managing costs and ensuring appropriate care.
The benefits of securing prior approval go beyond mere compliance; it helps in avoiding unexpected out-of-pocket expenses for patients. Additionally, it ensures that healthcare providers are reimbursed for the services rendered, which is vital for their practice's sustainability. Conversely, the absence of prior approval can lead to significant consequences such as delays in treatment, unexpected denials of claims, and, most importantly, adverse health outcomes for patients who may not receive the necessary care in time.
Step-by-step guide to completing the Nayzilam prior approval request form
Preparing to fill out the form
Before filling out the Nayzilam prior approval request form, it’s vital to gather all necessary documentation. This might include the patient's medical history, current medications, and previous treatment outcomes. A detailed understanding of the patient's condition and previous seizures will strengthen the request. Also, verifying patient eligibility, including checking insurance policy specifics, is essential to streamline the approval process.
Detailed instructions for each section of the form
Tips for submitting the Nayzilam prior approval request form
Choosing the right submission method is critical when it comes to the Nayzilam prior approval request form. Healthcare providers can opt for either online submissions or paper ones. Online submissions are typically quicker, allowing for immediate receipt confirmations, while paper submissions may face delays depending on mail service efficiency. Patients and providers should weigh the pros and cons based on their specific situations.
Best practices for ensuring approval include reviewing the completed forms thoroughly for any inaccuracies and double-checking specific requirements outlined by the patient's insurance provider. These steps can drastically reduce the risk of a denial and speed up the approval process.
Tracking your prior approval request
After submission, understanding the review process is crucial for both patients and healthcare providers. Generally, once the Nayzilam prior approval request form has been submitted, it enters a review phase where the insurance company evaluates the documentation provided. Depending on the insurance provider, this decision-making process can typically take anywhere from a few days to several weeks.
To effectively follow up, utilize direct methods such as phone calls or secure online message systems offered by many insurers. Document all interactions for reference, and do not hesitate to seek status updates if you do not receive feedback within the expected time frame.
Common reasons for denial and how to address them
Numerous factors can lead to denied claims for the Nayzilam prior approval request. These may include lacking sufficient medical justification, not adhering to the insurance policy guidelines, or submitting incomplete information. For example, cases where patients have incomplete treatment history documentation often face rejections, which can be disheartening.
However, denial isn't the end of the road. To appeal a denied request, it’s essential to understand the specific reasons cited by the insurer. Upon receipt of the denial notice, promptly follow the outlined appeals process, including drafting a comprehensive appeal letter that addresses each reason for denial and includes supporting documentation whenever possible.
Resources for assistance with the Nayzilam prior approval request form
Patient advocacy groups can play an invaluable role in guiding individuals through the complexities of the Nayzilam prior approval request form. Organizations often provide resources such as sample letters, FAQs, and even direct assistance through trained advocates who understand the nuances of navigating insurance processes.
Additionally, maintaining a list of key contacts within major insurance firms can also streamline communication as you seek approval. Insurance companies often have dedicated representatives who specialize in handling medication approvals, and leveraging these contacts can expedite your requests.
Conclusion remarks on the importance of effective document management
Effective document management is crucial in healthcare, especially when it comes to prior approvals like the Nayzilam request form. Utilizing platforms such as pdfFiller empowers users to seamlessly edit, sign, collaborate, and manage their documents from a single, cloud-based platform. This not only simplifies the process of managing approvals but also enhances the ability to keep accurate records over time.
Encouraging utilization of available tools like pdfFiller can significantly reduce the stress associated with document preparation, ensuring every submission is thorough and complete. Access to digitized, interactive resources allows for efficient tracking and management, paving the way for more successful healthcare outcomes.
Insights into the impact of effective prior approval on patient care
Securing prior approval for Nayzilam not only facilitates access to essential medication but also enhances the overall quality of care documents—leading to improved health and financial outcomes for patients. By understanding the intricacies of the prior approval process and managing documentation effectively, both patients and healthcare providers can ensure a more streamlined approach to treatment. Proper documentation is not merely a bureaucratic requirement; it's a vital aspect of delivering effective healthcare and ensuring patient safety.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit nayzilam prior approval request from Google Drive?
How can I edit nayzilam prior approval request on a smartphone?
How can I fill out nayzilam prior approval request on an iOS device?
What is nayzilam prior approval request?
Who is required to file nayzilam prior approval request?
How to fill out nayzilam prior approval request?
What is the purpose of nayzilam prior approval request?
What information must be reported on nayzilam prior approval request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.