Get the free Prescription Drug Prior Authorization Request
Get, Create, Make and Sign prescription drug prior authorization



How to edit prescription drug prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prescription drug prior authorization

How to fill out prescription drug prior authorization
Who needs prescription drug prior authorization?
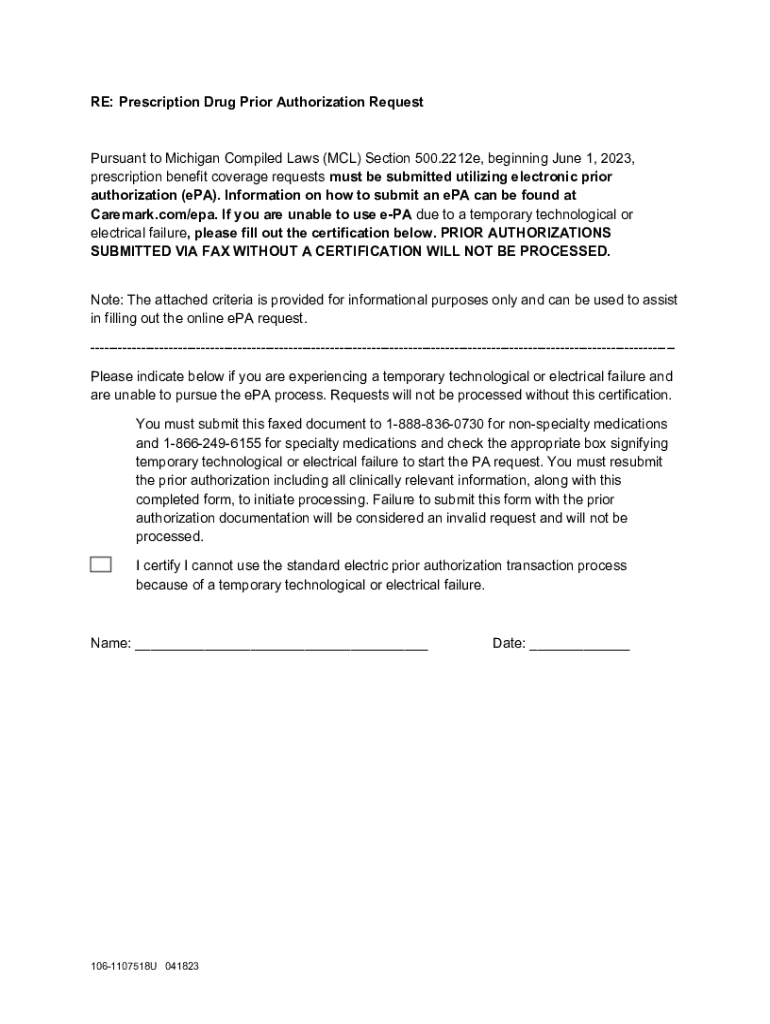
Understanding the Prescription Drug Prior Authorization Form
Understanding prescription drug prior authorization
Prior authorization is a process required by many insurance plans before covering specific medications or treatments. This mechanism ensures that the prescribed treatment is necessary and appropriate for the patient's condition. By requiring prior authorization, insurance companies aim to control healthcare costs without compromising patient care.
The importance of prior authorization extends beyond insurance savings; it plays a critical role in ensuring that patients receive the right medications tailored to their health conditions. Prior authorization also helps in minimizing the use of ineffective or unnecessary treatments, fostering better health outcomes.
Generally, medications that are costly, have lower efficacy, or that require a lengthy treatment process are subjected to prior authorization. This procedure supports a thorough examination of each case to ensure that decisions prioritize patient welfare.
The role of the prior authorization form
The prior authorization form serves as the standardized document through which healthcare providers request approval from insurers before a medication can be prescribed. This form contains essential information that justifies why a particular medication is necessary for a patient’s specific health condition.
Key components of the prior authorization form typically include patient demographics, medication details, prescribing provider information, and clinical justifications. An accurately filled form ensures that healthcare providers can make informed decisions while minimizing any administrative delays.
Completing the form incorrectly can lead to significant delays in medication access, ultimately compromising patient health outcomes. Precision in filling out this form is essential to facilitate a smooth authorization process.
Preparing to complete the prior authorization form
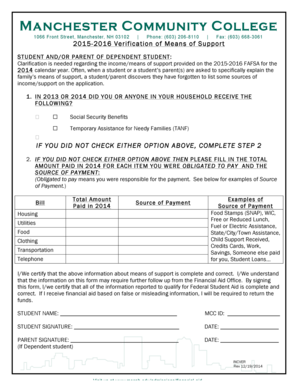
To effectively complete a prior authorization form, it is critical to gather necessary patient information ahead of time. This information includes the patient’s full name, date of birth, insurance policy details, and a comprehensive medication history that includes prior treatments and responses.
Many insurance providers have unique requirements regarding the prior authorization process. Before filling out the form, check specific guidelines provided by the patient’s insurance company. Understanding these requirements ensures that all necessary documentation is prepared, increasing the likelihood of a favorable response.
Gathering these details not only expedites form completion but also enhances the overall quality of the information provided to insurers.
Step-by-step guide to filling out the prescription drug prior authorization form
Filling out the prior authorization form can be straightforward if approached methodically. Here’s a breakdown of each step to ensure that the form is completed accurately:
Following this structured approach minimizes errors and ensures that all necessary information is provided for a successful authorization.
Submitting your prior authorization form
Once the prior authorization form is completed, the next step is submission. Insurers usually offer several methods for submitting the form, including electronic and physical options. Electronic submission through dedicated healthcare portals can expedite the approval process due to faster data entry and processing.
It's essential to obtain confirmation of the submission and keep a record of any correspondence with the insurance provider. Follow-up calls may be necessary to ensure that the request is being processed and to address any potential issues before they escalate.
Staying proactive in tracking the status of your submission can significantly affect the outcome and timing of the authorization decision.
Common challenges and solutions
Navigating the prior authorization process can be fraught with challenges. Common issues include denials, requests for additional information, and prolonged wait times. Understanding these obstacles helps patients and providers prepare accordingly.
One of the primary solutions to addressing denials is to ensure that the clinical justification must be compelling and well-supported by evidence from medical literature or previous treatment outcomes. In cases of incomplete information, always provide as much detail and documentation as possible.
Embracing these strategies can minimize the time and effort required to manage prior authorization issues effectively.
Managing the authorization process
Once a prior authorization form is submitted, managing the timeline for approval is crucial. Insurance companies usually have specific timeframes within which they must respond to a request, often ranging from a few days to a few weeks depending on the medication's complexity and insurer policies.
It is essential to remain vigilant for any signs of delays or problems, such as lack of communication from the insurer or request for additional documentation after submission, which can happen frequently.
Cultivating an understanding of the prior authorization process fosters patience and ensures timely medications.
Utilizing pdfFiller for your prior authorization needs
pdfFiller provides a robust platform designed to simplify the management of prior authorization forms. Users can easily access, fill, and edit the prescription drug prior authorization form from anywhere, streamlining the entire process.
One standout feature of pdfFiller is its ability to enable secure e-signatures and store documents in a centralized, cloud-based environment. This not only simplifies record-keeping but also promotes efficient collaboration among healthcare teams.
These capabilities not only enhance the overall experience but also lead to faster processing times for prior authorization requests.
Future of prior authorization in healthcare
The landscape of prior authorization is evolving, influenced by technological innovations in healthcare. Digital submissions, enhanced analytics, and automated processing are progressively shaping more efficient workflows.
As healthcare pushes towards being more patient-centered, advocacy groups and healthcare organizations are working tirelessly to streamline prior authorization requirements ensuring they are not a burden on patient care. Continued dialogue between patients, providers, and insurers fosters improvements.
Fostering a collaborative environment among stakeholders is essential for advancing the effectiveness of the prior authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find prescription drug prior authorization?
Can I create an electronic signature for the prescription drug prior authorization in Chrome?
How do I fill out the prescription drug prior authorization form on my smartphone?
What is prescription drug prior authorization?
Who is required to file prescription drug prior authorization?
How to fill out prescription drug prior authorization?
What is the purpose of prescription drug prior authorization?
What information must be reported on prescription drug prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.