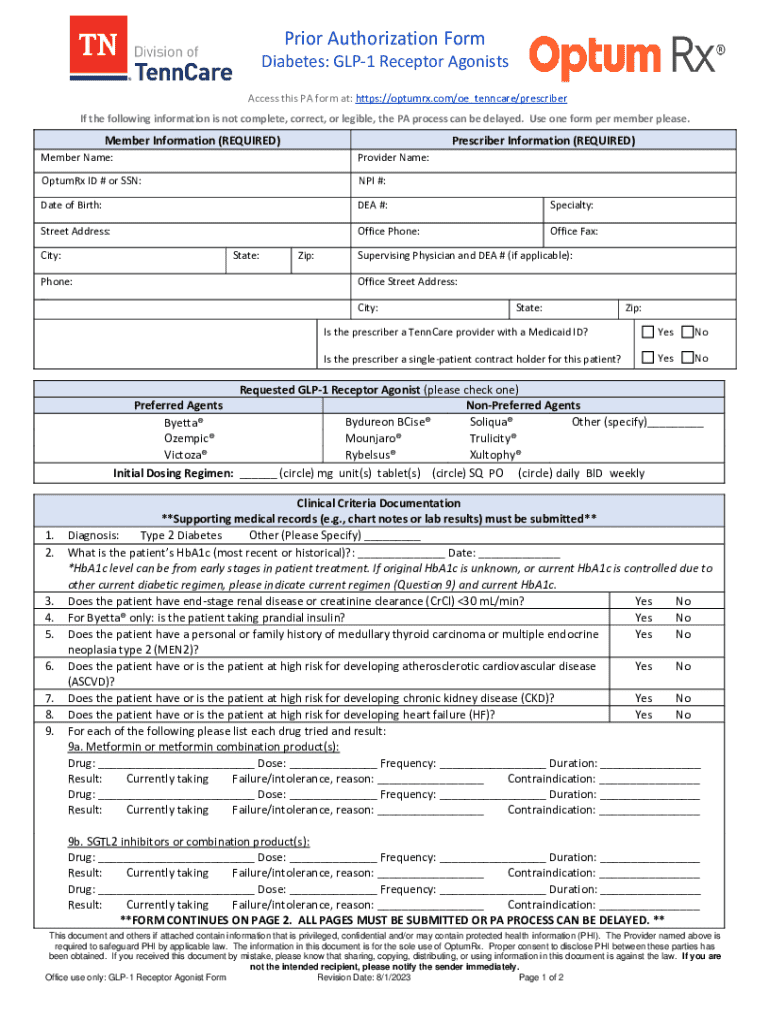
Get the free Prior Authorization Form
Get, Create, Make and Sign prior authorization form



How to edit prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization form

How to fill out prior authorization form
Who needs prior authorization form?
Prior Authorization Form: A Comprehensive How-to Guide
Understanding prior authorization
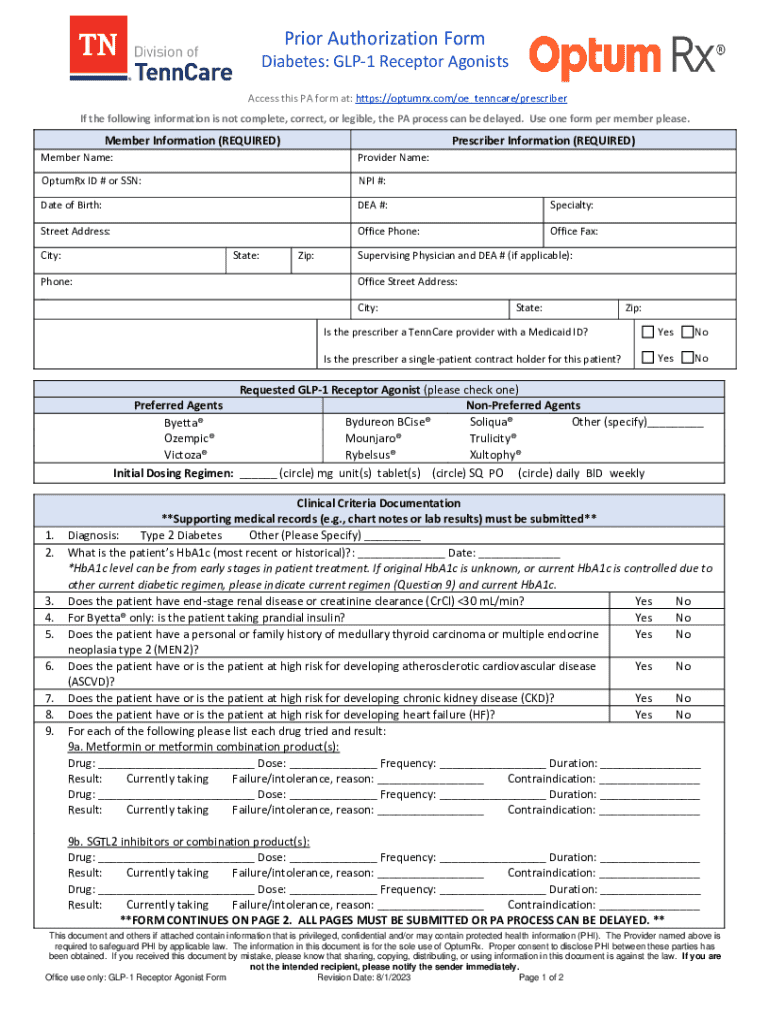
A prior authorization form is a crucial document in the healthcare landscape, serving as a gatekeeper to ensure that certain medical services, medications, or procedures are covered by insurance. This document, which is submitted by your healthcare provider, must be approved by your insurance company before the treatment can proceed. The importance of obtaining prior authorization lies not only in potential cost savings for patients but also in ensuring that the proposed treatment aligns with the insurer's medical necessity standards.
In many instances, prior authorization helps to control healthcare costs and prevent unnecessary procedures. Insurers use this process to verify that a treatment is appropriate and necessary based on established clinical guidelines. Understanding the role of prior authorization allows patients and healthcare providers to navigate the complexities of insurance coverage effectively.
When is prior authorization required?
Prior authorization is often required in various scenarios, such as when a patient is prescribed high-cost medications, undergoes certain surgical procedures, or receives advanced imaging services like MRIs or CT scans. These scenarios typically include examples like specialty drugs for chronic conditions, expensive diagnostic tests, or even inpatient admissions requiring prolonged stays at hospitals.
To give you a better idea, here are some common circumstances where a prior authorization form may be necessary:
Overview of the prior authorization process
The prior authorization process involves several key participants, each playing a vital role. Healthcare providers initiate the process by requesting approval for their recommended treatment on behalf of the patient. They must thoroughly document medical necessity, which is crucial for the insurance company's evaluation.
The insurance company then reviews the prior authorization form based on the submitted medical evidence. If the insurer determines that the requested treatment is medically necessary and adheres to their policies, approval is granted. Conversely, if they find discrepancies, they may deny the request or seek additional information from the healthcare provider.
Below are the typical steps involved in the prior authorization process:
Filling out the prior authorization form
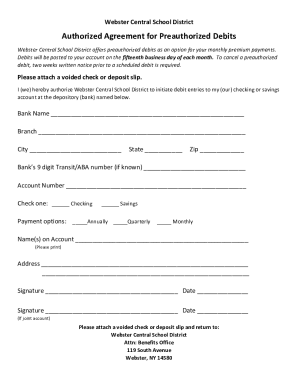
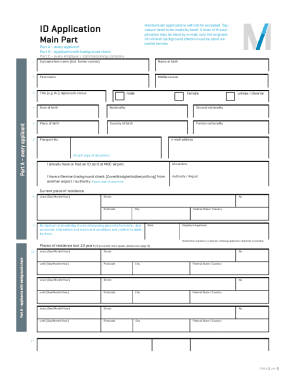
Completing a prior authorization form accurately is critical to ensure that there are no delays in treating patients. The essential information required on such forms generally includes patient details, provider specifications, and information about the requested treatment or medication.
Some specifics needed in the form typically include:
Here are step-by-step instructions to successfully complete the prior authorization form:
While filling out the prior authorization form, it's important to avoid common mistakes such as missing signatures or dates, providing incomplete patient or provider information, or neglecting to attach relevant medical documentation. These errors can not only delay the process but can also lead to outright denials.
Interactive tools and templates
Utilizing pdfFiller can ease the burden of managing prior authorization forms with its smooth document management solutions. With pdfFiller, users can easily access, edit, and customize prior authorization templates to fit specific needs. The platform’s features, like auto-fill and eSignature, streamline the form-filling process, ensuring accuracy and completeness.
Here’s how you can benefit from the tools provided by pdfFiller:
Additionally, pdfFiller offers great resources, tutorials, and FAQs related to using their platform's functionalities and managing prior authorizations effectively. Utilizing these interactive tools can save time and prevent common pitfalls during the documentation process.
Managing submitted prior authorization requests
Once a prior authorization request is submitted, it's essential to understand what happens next in the review process. Generally, health insurance companies will have specific timelines for reviewing submitted forms. Familiarizing yourself with these timelines can help set expectations and follow up appropriately.
Tracking the status of your request can be done conveniently with pdfFiller. The platform allows users to manage submissions and access status updates efficiently. Following up proactively can make a significant difference in case you need to provide any additional information or clarification.
If a request is denied, it's important to remain calm and take the necessary steps to appeal the decision. First, gather all documentation that supports medical necessity, which will be crucial in disputing the denial. Prepare a clear, concise appeal that addresses the specific reasons for denial and provide all necessary supporting evidence to strengthen your case.
Tips for successful prior authorization
Successful prior authorization often hinges on effective communication with your healthcare provider. It is crucial to keep your provider informed about any changes in your health status or medication needs that may necessitate a new request. Establish a channel of ongoing dialogue to ensure that any changes are reported promptly, allowing for a smoother submission process.
Taking proactive steps ahead of time can also streamline the prior authorization process. Keeping organized records of prior authorizations, including documentation, outcomes, and dates, is invaluable in maintaining a comprehensive view of your healthcare journey. This can not only facilitate future submissions but also assist your healthcare provider in making informed decisions regarding your treatment options.
Frequently asked questions (FAQs)
General questions about prior authorization
Patients often wonder about the average turnaround time for approval of a prior authorization request. This timeframe can vary significantly based on the insurer; however, typical responses may take anywhere between 24 to 72 hours if all information is complete. Knowing your insurer's specific process can aid in managing expectations.
To expedite the process, ensure that all required documentation and information are submitted in one go to prevent back-and-forth communications that can delay approval.
Specific questions related to using pdfFiller
Users of pdfFiller often inquire about how to save and store completed forms securely. The platform offers a cloud-based solution with secure access that lets you keep your documents organized and protected. Furthermore, if multiple users need to collaborate on a prior authorization form, pdfFiller’s features make it easy to invite team members for real-time editing and adjustments, enhancing collaboration at every step.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in prior authorization form?
How can I edit prior authorization form on a smartphone?
How do I complete prior authorization form on an Android device?
What is prior authorization form?
Who is required to file prior authorization form?
How to fill out prior authorization form?
What is the purpose of prior authorization form?
What information must be reported on prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.