Get the free Evrysdi Prior Authorization Request Form
Get, Create, Make and Sign evrysdi prior authorization request
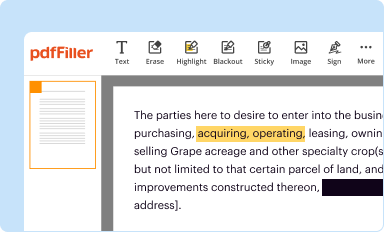
How to edit evrysdi prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out evrysdi prior authorization request
How to fill out evrysdi prior authorization request
Who needs evrysdi prior authorization request?
Evrysdi Prior Authorization Request Form: A Comprehensive Guide
Understanding Evrysdi and its importance
Evrysdi (Risdiplam) is an oral medication designed for the treatment of spinal muscular atrophy (SMA), a genetic disorder that affects motor neuron cells in the spinal cord. By enhancing the production of SMN protein, Evrysdi plays a crucial role in improving muscle function and overall quality of life for patients, especially children. Given its significance in managing SMA, prior authorization becomes vital in ensuring that patients can access this necessary treatment without unnecessary delays or financial burdens.
Prior authorization acts as a safeguard in the healthcare system, requiring healthcare providers to obtain approval from insurance companies before the medication can be dispensed. This process validates the medical necessity and appropriateness of the treatment based on individual patient needs. Securing prior authorization not only affirms the medical necessity but also alleviates concerns regarding out-of-pocket costs for patients and families.
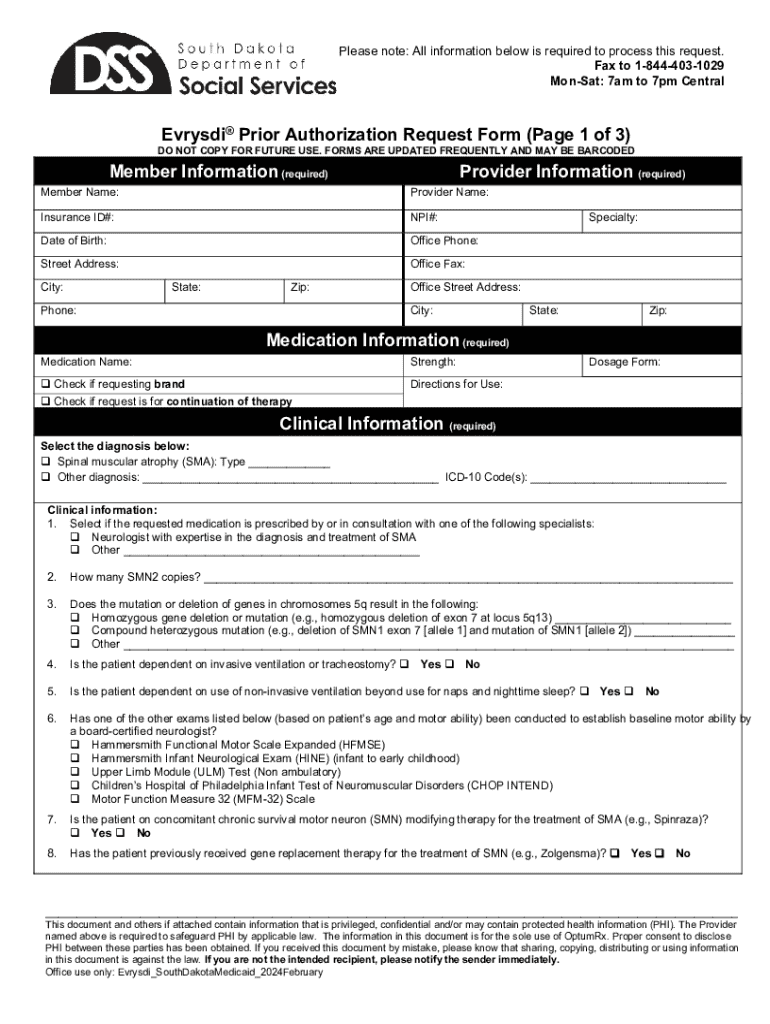
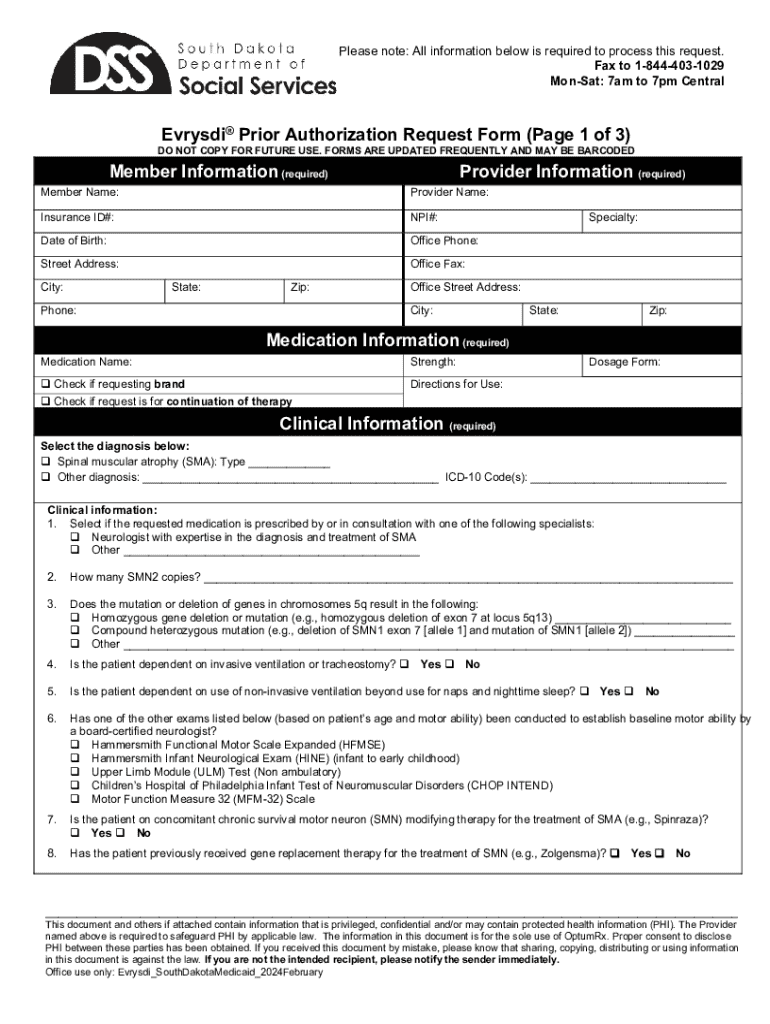
Key information required for the prior authorization request
When filling out the Evrysdi prior authorization request form, specific patient details must be included to ensure the process can move forward smoothly. Essential information such as patient demographics, including name, birth date, and insurance details, are critical starting points. Each piece of data plays a role in establishing the patient's identity and insurance coverage for the medication.
Additionally, comprehensive clinical history relevant to the treatment must be thoroughly documented. Details should encompass previous treatment regimens, any responses to those treatments, and current health status which might justify the necessity of Evrysdi. Furthermore, attaching pertinent documentation such as previous treatment records, medical imaging, and a physician’s prescription with rationale strengthens the request.
Step-by-step guide to filling out the Evrysdi prior authorization request form
Filling out the Evrysdi prior authorization request form can be a straightforward process when properly organized. Here’s a step-by-step guide to ensure that all necessary information is captured accurately.
Step 1: Gather necessary documentation
Begin by gathering all required documents, which should include patient identification details, previous treatment records, and a prescription from the healthcare provider. Organizing these documents ahead of time will streamline the subsequent steps.
Step 2: Complete patient information section
In the patient information section, accurately fill in personal details such as the patient’s full name, date of birth, and insurance information. Ensure correct spelling and format, as any discrepancies can lead to delays.
Step 3: Provide clinical information
Summarize the clinical history, including prior treatments and responses. This section should detail any medications previously used, treatment regimens, and the outcomes of those treatments to substantiate the case for Evrysdi.
Step 4: Fill out health insurance information
Accurately document the health insurance details of the patient. Highlight key aspects such as the policy number, group number, and any co-pay or deductible amounts that may be relevant to the approval process.
Step 5: Attach supporting documents
When ready to submit, ensure all supporting documents are attached to the request form. This includes copies of previous treatment records, clinical notes, and the physician's prescription with a clear justification for prescribing Evrysdi.
Step 6: Final review of the request form
Conduct a thorough final review before submission. Utilize a checklist to ensure all necessary items are included and correctly filled out. Mistakes or missing information at this stage can significantly delay the authorization process.
Common mistakes to avoid in the prior authorization process
Even with the best intentions, many patients and providers encounter pitfalls during the prior authorization process for Evrysdi. Common mistakes range from incomplete patient information to missing supporting documents. Such errors can result in unnecessary delays, increasing the frustration for patients in urgent need of their medication.
It’s vital to emphasize the importance of clarity and accuracy in every section of the form. Providing vague or unclear patient histories or clinical justifications can lead to a lack of understanding from the insurer's side, resulting in denials. Ensuring all documentation is correct and complete helps expedite the review process.
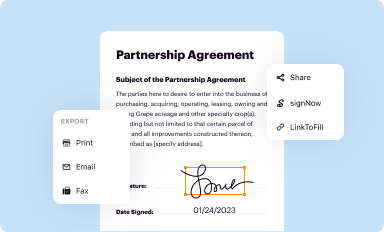
Submitting the prior authorization request
Once the prior authorization form is complete, the next step is submission. There are several methods by which the request can be submitted, including electronic submissions or traditional paper forms. Each method has its own protocols depending on the insurer.
After submission, it's crucial to follow up on the request status. Insurers may have varied turnaround times for authorization, typically influenced by the method of submission. Online submissions often lead to quicker processing times compared to paper forms. Keep diligent records of all communications and a timeline of the submission to ensure an effective follow-up.
Dealing with denials
If a prior authorization request for Evrysdi is denied, understanding the common reasons can help in formulating an effective appeal. Denials may occur due to lack of medical necessity justification, incomplete submissions, or outdated clinical information. Recognizing these points can streamline the re-application process.
To appeal a denied request, start by crafting a compelling appeal letter. This letter should directly address the reason for the denial, refuting the insurer's claims with robust evidence and a detailed explanation. Gathering additional evidence, such as updated medical records or specialist recommendations, further strengthens the case.
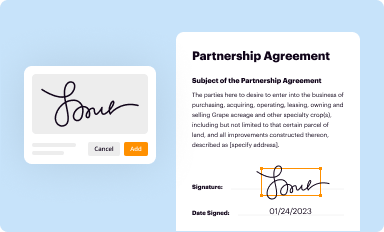
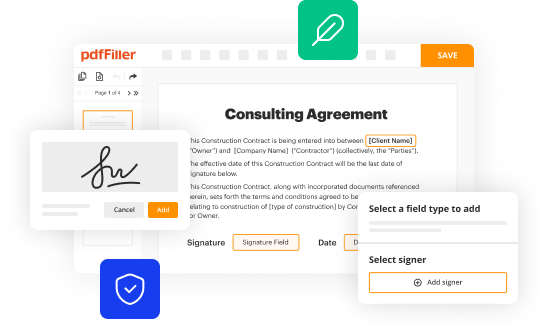
Utilizing pdfFiller for document management
Efficient document management is crucial during the prior authorization process, and pdfFiller emerges as a notable ally for both patients and healthcare providers. This cloud-based platform allows users to edit the Evrysdi prior authorization request form swiftly and effectively, ensuring that all necessary information is captured.
pdfFiller's features significantly enhance document handling. Users can edit and fill forms online seamlessly, sign documents electronically for expedited approvals, and collaborate with healthcare teams to gather necessary input. Additionally, accessing forms from anywhere ensures that the entire prior authorization process is managed with ease.
Frequently asked questions about Evrysdi prior authorization
After submitting the prior authorization request for Evrysdi, many patients wonder what the next steps entail. Typically, after submission, the insurer will review the request, and a determination will be communicated within a specified timeframe, which can vary based on the insurer and submission method. In cases where urgent timelines are crucial, patients should discuss this with their healthcare provider to mark urgency on their request.
If approval is denied, patients can explore alternatives depending on their clinical history and insurance policies. Alternative treatments may exist, but discussing options with healthcare providers is essential to ensure continuity of care.
Testimonials and success stories
Many patients have successfully navigated the Evrysdi prior authorization process, highlighting the importance of thorough preparation and effective communication. For instance, families have reported positive outcomes after ensuring all necessary documentation was perfectly in order, leading to swift approvals. The use of tools like pdfFiller has played a pivotal role in these success stories, allowing seamless collaboration and timely submissions with reduced stress.
These real-life experiences underscore the effectiveness of comprehensive document management and reinforce the potential for positive outcomes when pursuing prior authorization. Other families may be inspired by these testimonials, knowing that with the right tools and approach, overcoming bureaucratic hurdles is achievable.
Conclusion: Empowering your document management experience
In conclusion, the Evrysdi prior authorization request process can be navigated successfully with careful planning and thorough documentation. Utilizing solutions like pdfFiller not only streamlines the form-filling process but also empowers users to manage their documents effectively from anywhere. By leveraging its features, patients and providers can ensure timely and accurate submissions, thus facilitating quicker access to critical medications.
By embracing a comprehensive document management strategy, individuals can simplify the complexity of healthcare processes, ensuring that they receive the care and medications they need without unnecessary delays.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send evrysdi prior authorization request to be eSigned by others?
Can I create an eSignature for the evrysdi prior authorization request in Gmail?
How can I fill out evrysdi prior authorization request on an iOS device?
What is evrysdi prior authorization request?
Who is required to file evrysdi prior authorization request?
How to fill out evrysdi prior authorization request?
What is the purpose of evrysdi prior authorization request?
What information must be reported on evrysdi prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.