Get the free Prior Authorization Request Form
Get, Create, Make and Sign prior authorization request form
Editing prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form
How to fill out prior authorization request form
Who needs prior authorization request form?
Everything You Need to Know About the Prior Authorization Request Form
Understanding prior authorization
Prior authorization is a crucial process in the healthcare system, designed to ensure that prescribed procedures, medications, or treatments are medically necessary and covered by insurance before they are administered. Insurers require prior authorization to filter out unnecessary services and to control healthcare costs, ultimately safeguarding both the provider and the patient.
The importance of prior authorization cannot be overstated. It protects patients from unexpected medical expenses and equips healthcare providers with the necessary approvals to proceed with care. Key stakeholders in this process predominantly include healthcare providers, insurance companies, patients, and sometimes, pharmacy benefit managers. Misunderstandings or mistakes in the prior authorization request can lead to denied claims, delaying treatment or services, so it's vital to navigate this process diligently.
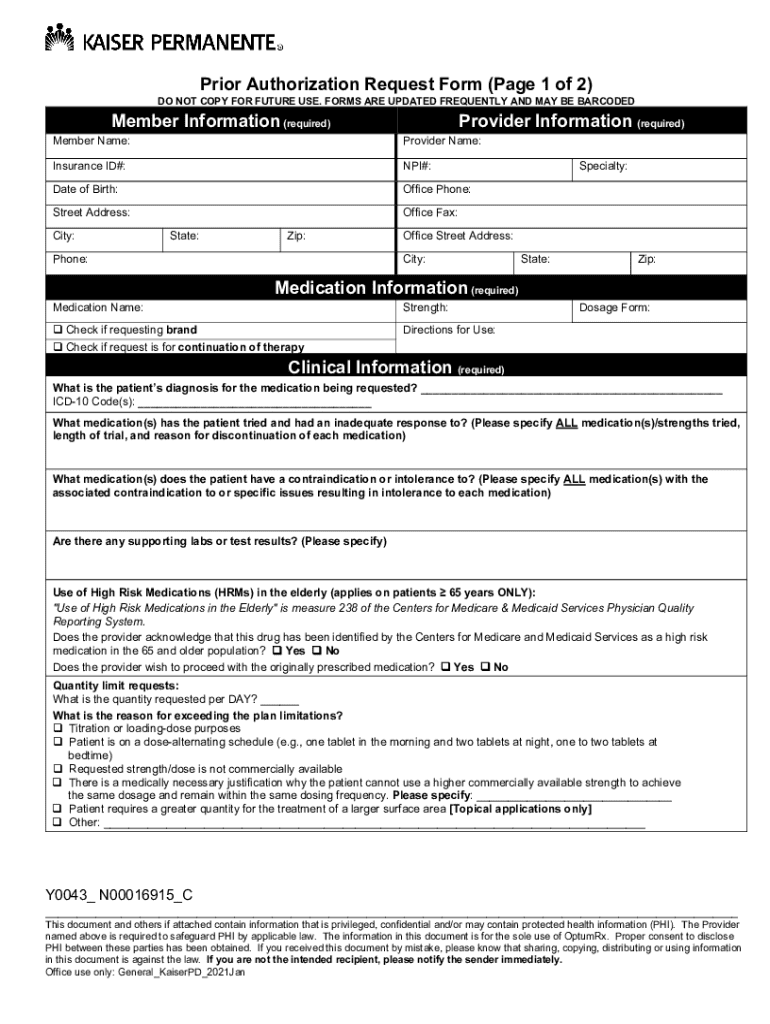
Overview of the prior authorization request form
The prior authorization request form serves a crucial purpose: it establishes the medical necessity of a treatment or medication that patients may need. Without this form, healthcare providers cannot efficiently secure coverage, impacting patients' access to timely care. The essential components of the form typically include patient information, provider details, treatment or medication specifics, insurance information, and additional supporting documentation.
Insurance providers may present different requirements for their prior authorization forms. It's vital to be aware of these differences, as each insurance company may ask for varied information or supporting documents. Understanding these distinctions allows for a more tailored request, increasing the chances of approval on the first submission.
How to access the prior authorization request form
Accessing the prior authorization request form is generally straightforward. Most insurance companies house these forms on their official websites, easily accessible for providers and patients alike. Additionally, pdfFiller provides a specialized platform to search for and retrieve these forms quickly, streamlining the entire process.
Users can choose between paper and digital versions of the form. While many prefer the digital format for its convenience, having a physical copy can be beneficial in settings where electronic access is limited. pdfFiller enhances accessibility by enabling users to fill out forms directly in their browsers, sidestepping cumbersome downloads or printouts.
Detailed step-by-step instructions for filling out the form
Section 1: Patient information
In this section, vital details include the patient's full name, date of birth, address, and insurance policy number. Common pitfalls here include entering incorrect birth dates or misplacing insurance information, which can lead to unnecessary delays.
Section 2: Provider information
Providers must accurately provide their name, contact information, and NPI (National Provider Identifier) number, which is essential for verification with insurance companies. Double-checking these details ensures smooth processing of the request.
Section 3: Procedure or medication information
This section must specify the procedure or medication in question, including the relevant codes (like CPT or HCPCS codes for procedures). Clearly documenting why the treatment is necessary can significantly enhance the request's approval chances.
Section 4: Insurance details
It's crucial to include the insurance policy number, group number, and contact details for the insurance company. Inaccuracies in this section can lead to processing delays or denials.
Section 5: Supporting documentation
Supporting documentation might include medical records, previous treatment details, or any relevant test results that substantiate the necessity of the requested treatment or medication. Including comprehensive documents can greatly impact the approval process.
Step 6: Reviewing your submission
Before submitting the request, reviewing is crucial. Create a checklist that includes verifying patient and provider details, ensuring all necessary supporting documentation is attached, and confirming that no sections of the form are left blank.
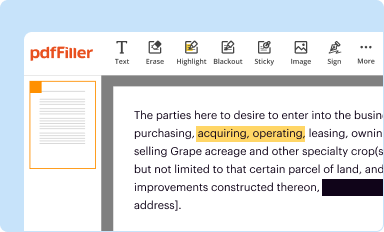
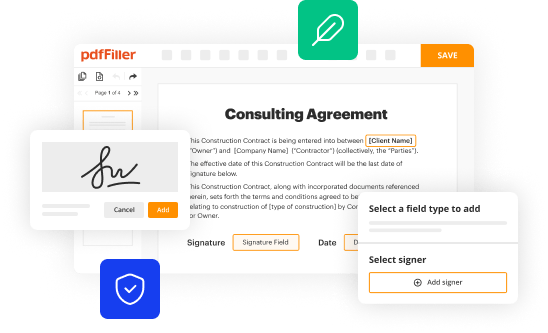
Editing and managing your form using pdfFiller
pdfFiller makes it easy to edit the prior authorization request form online. Users can navigate the interactive interface to input information without hassle. This platform not only allows for editing but also incorporates features like form templates, making the process much more efficient.
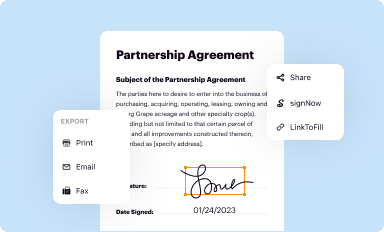
The ability to save and export completed forms directly from pdfFiller is a game-changer. Users can easily share their documents, whether for collaboration with colleagues or for submission to insurance companies, significantly reducing the administrative workload.
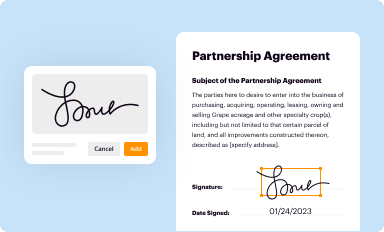
Signing and sending your prior authorization request
The digital signing process offered by pdfFiller is seamless and secure. Users can easily eSign their completed forms without the need for physical paperwork, which also ensures that all documentation adheres to legal standards.
When submitting your form, best practices include double-checking submission guidelines outlined by the insurance provider, such as acceptable file formats and submission methods, to avoid unnecessary complications. After submission, tracking the request is crucial, as it aids in following up and ensures that you remain informed about the status.
Common challenges and solutions in the prior authorization process
Delays in approval can arise for various reasons, including incomplete documentation or high volumes of requests at the insurance company. It's advisable to maintain open communication with insurance representatives to expedite the process. To prevent such issues, ensuring that all required documents are submitted accurately at the outset can save time.
In the event that a request is denied, understanding the reasons provided by the insurer can help in formulating a strong appeal. Gathering additional supporting evidence and rephrasing your justification can often turn the tide in these situations.
Frequently asked questions (FAQs)
What happens if a prior authorization is not obtained? Proceeding without prior authorization can result in the denial of coverage, leaving patients responsible for the full cost of treatment. Thus, it is essential to obtain this approval beforehand.
How long does the prior authorization process take? Typically, the process may vary depending on the insurance provider, but it generally takes anywhere from a few days to several weeks. It’s crucial to remain proactive during this waiting period.
Can multiple requests be submitted simultaneously? While it is possible to submit multiple requests, it's essential to ensure that each is complete and that you are careful not to overlap any information, as this can lead to confusion during processing.
Conclusion: maximizing efficiency and success in your prior authorization requests
In summary, successfully navigating the prior authorization request form requires thoroughness and attention to detail. By adhering to best practices outlined in this guide, you can streamline your submissions and enhance the chances of approval.
Utilizing pdfFiller for ongoing document management not only simplifies form completion but also bolsters collaboration across teams. With its cloud-based platform, you can manage all your documentation needs, enhancing efficiency in healthcare environments.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out the prior authorization request form form on my smartphone?
Can I edit prior authorization request form on an iOS device?
How can I fill out prior authorization request form on an iOS device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.