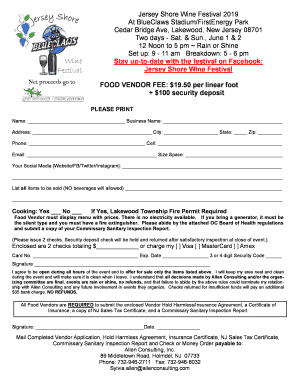
Get the free Prior Authorization Request Prescriber Fax
Get, Create, Make and Sign prior authorization request prescriber
Editing prior authorization request prescriber online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request prescriber
How to fill out prior authorization request prescriber
Who needs prior authorization request prescriber?
Prior Authorization Request Prescriber Form: A Complete Guide
Understanding prior authorization
Prior authorization is a critical process in the healthcare system that requires healthcare providers to obtain approval from insurance companies before providing specific treatments, medications, or procedures. This step is essential for ensuring that treatments are not only necessary but also covered by the patient's insurance plan. The importance of prior authorization stems from its role in controlling costs and ensuring that appropriate care is delivered to patients.
The impact of prior authorization on patient care is significant. Delays in gaining approval can lead to postponed treatments, creating barriers to timely patient care. Patients may experience frustration and uncertainty during this process, which can adversely affect their health outcomes. Therefore, understanding the stakeholders involved, including insurance companies, healthcare providers, and patients, is foundational to navigating the prior authorization process effectively.
Key elements of the prior authorization request prescriber form
When filling out a prior authorization request prescriber form, certain key elements must be included to ensure it is complete and processable. The required information typically consists of the following:
Additionally, supporting documents may be required to substantiate the request and include clinical notes, previous treatment history, and any relevant lab results. These documents help provide a comprehensive view of the patient's medical history and the rationale for the prescribed treatment.
Step-by-step instructions for filling out the form
Filling out the prior authorization request prescriber form can seem daunting, but a structured approach can simplify the process. Here’s a detailed guide to help you:
Paying close attention to these details will help ensure that your prior authorization request is submitted without any hiccups.
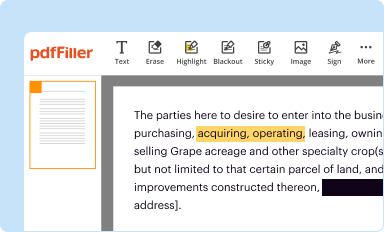
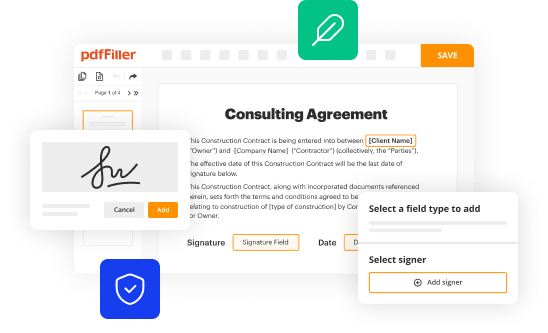
Editing and managing the form using pdfFiller
Once you have the prior authorization request prescriber form completed, using pdfFiller can enhance your document management experience. Here's how to effectively utilize this platform:
pdfFiller’s cloud-based platform streamlines the editing and collaboration process, making it easier to manage essential documents efficiently.
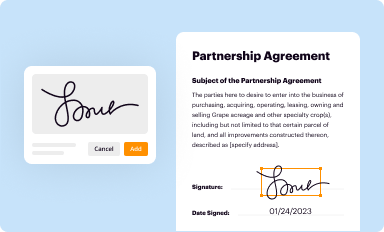
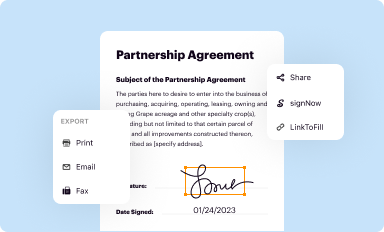
eSigning the prior authorization form
An important step in finalizing your prior authorization request is the eSignature. Here’s why it’s crucial and how to complete this step using pdfFiller:
Using electronic signatures expedites the process of submitting prior authorization requests, which can lead to faster approvals.
Submitting the prior authorization request
After completing and signing the prior authorization request prescriber form, it is time to submit it. Here’s how this can be managed efficiently:
These steps help ensure that your request for prior authorization is submitted accurately and monitored effectively.
Troubleshooting common challenges
Navigating the prior authorization process can present various challenges. Here are some common issues and how to address them:
Proactively addressing these challenges will make the prior authorization process smoother and more efficient.
Best practices for effective prior authorization management
To optimize the prior authorization process, implementing best practices is important. Here are some strategies that can enhance efficiency and ensure effectiveness:
By deploying these best practices, healthcare teams can improve their interaction with the prior authorization process, ultimately benefiting patient care.
Frequently asked questions
Despite being a routine part of patient care, prior authorization can be confusing. Here are some frequently asked questions that address common concerns:
These FAQs provide clarity and assist healthcare providers in navigating the challenges associated with prior authorization requests more effectively.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my prior authorization request prescriber in Gmail?
How can I edit prior authorization request prescriber on a smartphone?
How do I edit prior authorization request prescriber on an Android device?
What is prior authorization request prescriber?
Who is required to file prior authorization request prescriber?
How to fill out prior authorization request prescriber?
What is the purpose of prior authorization request prescriber?
What information must be reported on prior authorization request prescriber?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.