Get the free Utah Medicaid Pharmacy Prior Authorization Request Form
Get, Create, Make and Sign utah medicaid pharmacy prior



How to edit utah medicaid pharmacy prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out utah medicaid pharmacy prior

How to fill out utah medicaid pharmacy prior
Who needs utah medicaid pharmacy prior?
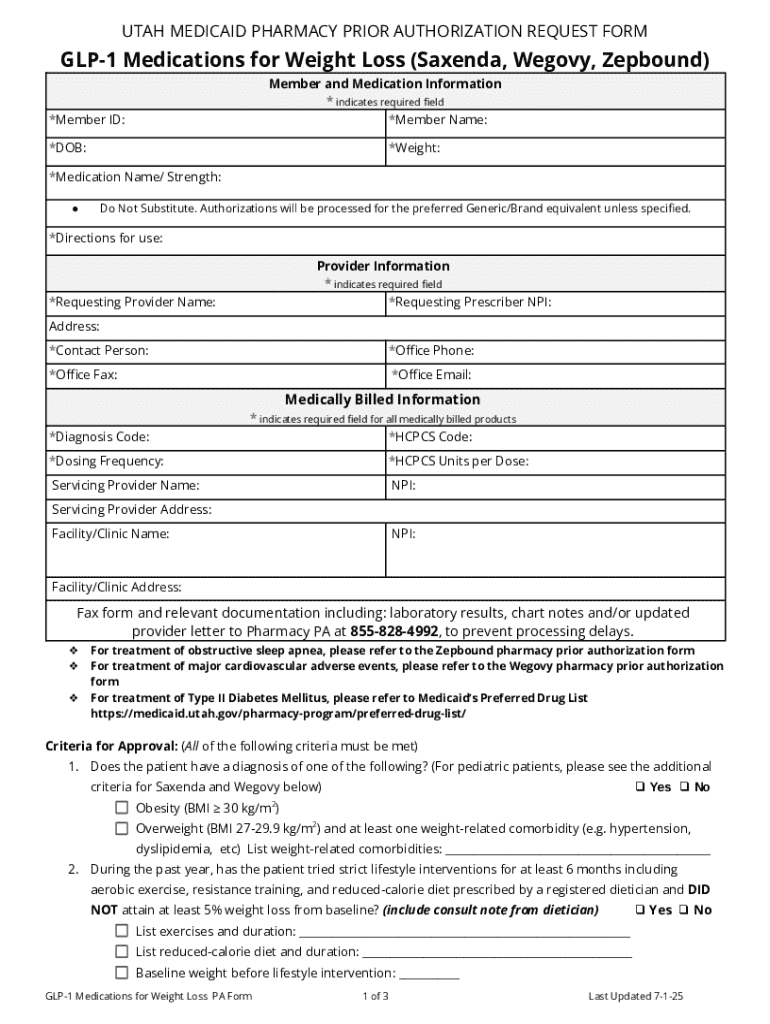
Understanding the Utah Medicaid Pharmacy Prior Form
Understanding Utah Medicaid pharmacy prior authorization
Prior authorization is a crucial component of Medicaid pharmacy services in Utah, designed to ensure that prescribed medications meet medical necessity criteria and are used effectively for patients. It involves obtaining approval from the Medicaid program before a medication can be dispensed, thereby ensuring that costs are justified and that patients receive suitable treatments.
The importance of prior authorization lies in its role in controlling medication costs and ensuring patient safety. By requiring healthcare providers to provide justification for specific medications, the Utah Medicaid program can encourage the use of more cost-effective choices and monitor utilization patterns to prevent overuse or misuse.
Eligibility criteria for Medicaid pharmacy prior authorization
Eligibility for Medicaid pharmacy services in Utah is primarily based on income level, age, and disability considerations. To qualify for Utah Medicaid, individuals must typically fall within specific income thresholds defined by the federal poverty level. Additionally, special attention is given to age groups, particularly children and the elderly, as well as those with disabilities who may have unique healthcare needs.
Certain conditions often necessitate prior authorization for pharmacy services. These may include chronic illnesses such as diabetes, hypertension, and asthma, which often require specialized treatments or medications. Medications that do not have established guidelines for use may also fall under this requirement, as Medicaid seeks to manage spending on specialty drugs and ensure they are used appropriately.
The prior authorization process in Utah
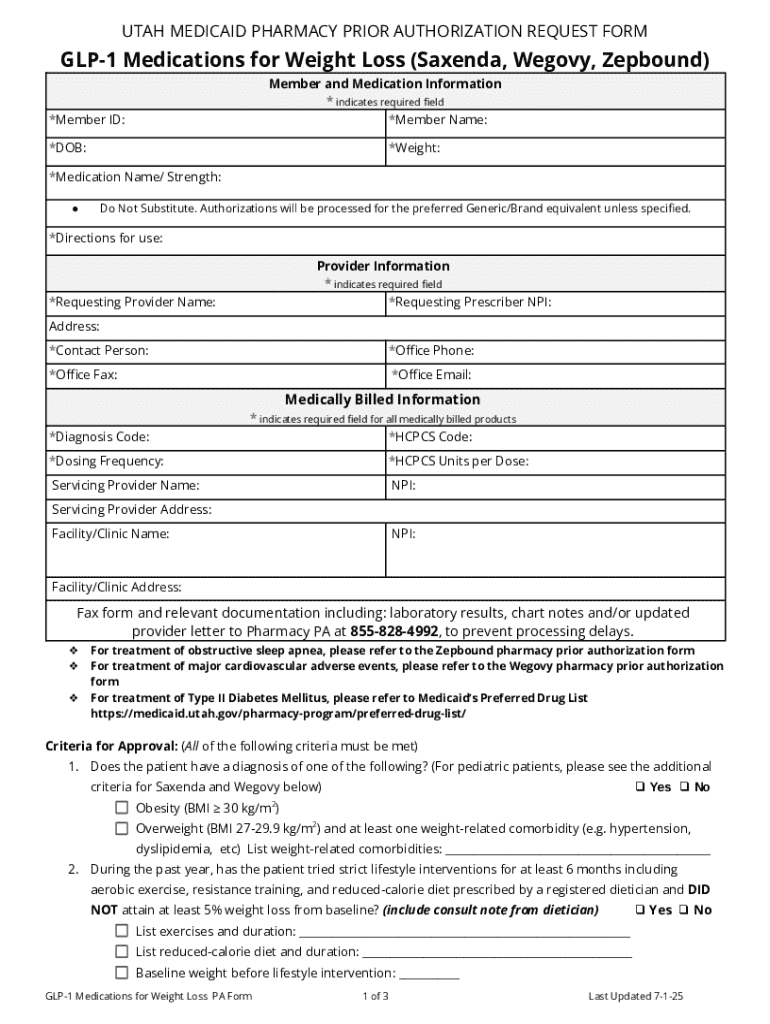
Navigating the prior authorization process can seem daunting, but understanding the steps can simplify it greatly. The process generally consists of four critical steps. First, healthcare providers must identify the medication that requires authorization. Next, they should gather essential patient information, including medical history and provider details. Following this, the Utah Medicaid pharmacy prior form needs to be completed accurately, encompassing all required data.
The final step involves submitting the request to the appropriate entity within the Utah Medicaid framework. Timeliness is crucial; providers need to be aware of specific timelines and deadlines for submission, as delays can impact the patient's access to medication. Post-submission, the provider will receive notification regarding the approval or denial of the request, at which point further action can be taken accordingly.
Required documentation for prior authorization
The Utah Medicaid pharmacy prior form requires several key components to be completed comprehensively. Essential details include patient demographics (name, date of birth, Medicaid ID), the prescriber's information (name, NPI number, contact details), and specific medication details such as drug name, dosage, and frequency of administration. Ensuring that all fields are filled accurately can potentially reduce processing time.
In addition to the form itself, providers may also need to attach supporting documents. These can include medical records that justify the necessity of the medication or details of previous treatments. Previous treatment history may showcase ineffective medications, underscoring the need for the proposed therapy. Having comprehensive documentation ready can facilitate a smoother authorization process.
Reviewing pharmacy criteria forms
Understanding the pharmacy criteria used for prior authorization in Utah is essential for healthcare providers. These criteria outline the circumstances under which specific medications may be authorized, helping to establish a framework for medication prescriptions. Common drugs requiring prior authorization often include high-cost medications, particularly those used for complex or chronic conditions.
In Utah, justifications required for authorization may vary from drug to drug. For example, medications for chronic pain management may require documentation outlining other treatment modalities attempted and their outcomes. Knowing the specifics of these criteria helps providers prepare robust authorization requests, increasing the likelihood of approval.
FAQs about Utah Medicaid pharmacy prior authorization
Many questions arise around the Utah Medicaid pharmacy prior authorization process. A common inquiry is about the duration it takes to obtain prior authorization; typically, responses are provided within 10 business days. However, complexity and completeness of the request can influence this timeline. In cases of denial, providers can appeal the decision, allowing for a reassessment based on additional information or alternative justifications.
It is beneficial for providers to follow best practices when submitting prior authorization requests. This includes ensuring all documentation is complete and accurate, adhering to submission guidelines, and maintaining open communication with the pharmacy benefit manager to address any queries that may arise during the review process.
Resources for patients and providers
Patients and providers seeking additional information about Utah Medicaid pharmacy services can benefit significantly from the available resources. The Utah Medicaid website provides comprehensive details about eligibility requirements, covered services, and the prior authorization process. Furthermore, dedicated support lines are available for providers needing immediate assistance regarding prior authorization submissions.
Local pharmacies often serve as invaluable resources and can provide information about specific medications and the prior authorization process. Training materials aimed at healthcare providers are also accessible, offering insights into best practices in document management and completing the prior authorization form accurately.
Maintaining compliance and managing medications
Remaining compliant with Medicaid's evolving policies is critical for sustainable pharmacy practice. Keeping informed about potential changes to prior authorization requirements and processes helps providers effectively manage their patients' medications and avoid delays in treatment. Staying proactive ensures adherence to Medicaid guidelines and ultimately contributes to better patient outcomes.
Tracking authorized medications can be challenging, particularly for patients with multiple health conditions requiring various treatments. Providers should encourage patients to maintain a detailed log of prescribed medications and any required prior authorizations. This practice not only helps in managing medications but also serves as a safeguard against discrepancies in treatment that could hinder recovery.
Best practices for utilizing the Utah Medicaid pharmacy prior form
To ensure efficient completion of the Utah Medicaid pharmacy prior form, healthcare providers should adopt specific best practices. Firstly, thoroughly reviewing all sections of the form beforehand can preemptively address any mistakes or omissions. Utilizing technology, such as document management solutions like pdfFiller, can simplify the process of filling out, editing, and signing the form electronically.
pdfFiller's features enhance collaborative efforts among healthcare teams, allowing for document sharing and real-time updates. By using tools for electronic signatures and cloud storage, providers can streamline the submission process, ensuring that all forms are filed promptly and correctly, leading to improved outcomes in obtaining prior authorizations.
Ongoing updates and changes to Medicaid pharmacy programs
Legislative changes affecting prior authorization processes can occur frequently, impacting both providers and patients. Staying updated on recent changes ensures that everyone involved understands the current requirements and standards that govern Medicaid pharmacy benefits. Healthcare professionals are encouraged to regularly check for announcements or updates from the Utah Medicaid program to stay informed on how these changes might influence their practice.
Looking ahead, providers and patients alike can expect refinements in the Medicaid pharmacy programs aimed at improving access and efficiency. Keeping an eye on ongoing developments in this area will foster a more effective healthcare system, and using platforms such as pdfFiller can aid in managing and adapting to these changes smoothly.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I execute utah medicaid pharmacy prior online?
How do I edit utah medicaid pharmacy prior online?
Can I create an electronic signature for signing my utah medicaid pharmacy prior in Gmail?
What is utah medicaid pharmacy prior?
Who is required to file utah medicaid pharmacy prior?
How to fill out utah medicaid pharmacy prior?
What is the purpose of utah medicaid pharmacy prior?
What information must be reported on utah medicaid pharmacy prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.