Get the free Prior Authorization Request Form
Get, Create, Make and Sign prior authorization request form



How to edit prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
Prior Authorization Request Form - How-to Guide
Understanding prior authorization
Prior authorization is a critical component of the healthcare system that requires healthcare providers to obtain approval from insurers before proceeding with certain medical treatments, procedures, or medications. This process is designed to ensure that the requested services are medically necessary and align with the patient's specific health needs. For patients, obtaining prior authorization can be a crucial step in accessing necessary care without unforeseen costs. Providers, on the other hand, must navigate these requirements to ensure timely treatment for their patients.
Key players in this ecosystem include insurers who create the policies, healthcare providers who request the authorizations, and patients who seek care. Understanding the roles of each is essential to navigating the prior authorization process effectively.
Before you begin: essential preparations
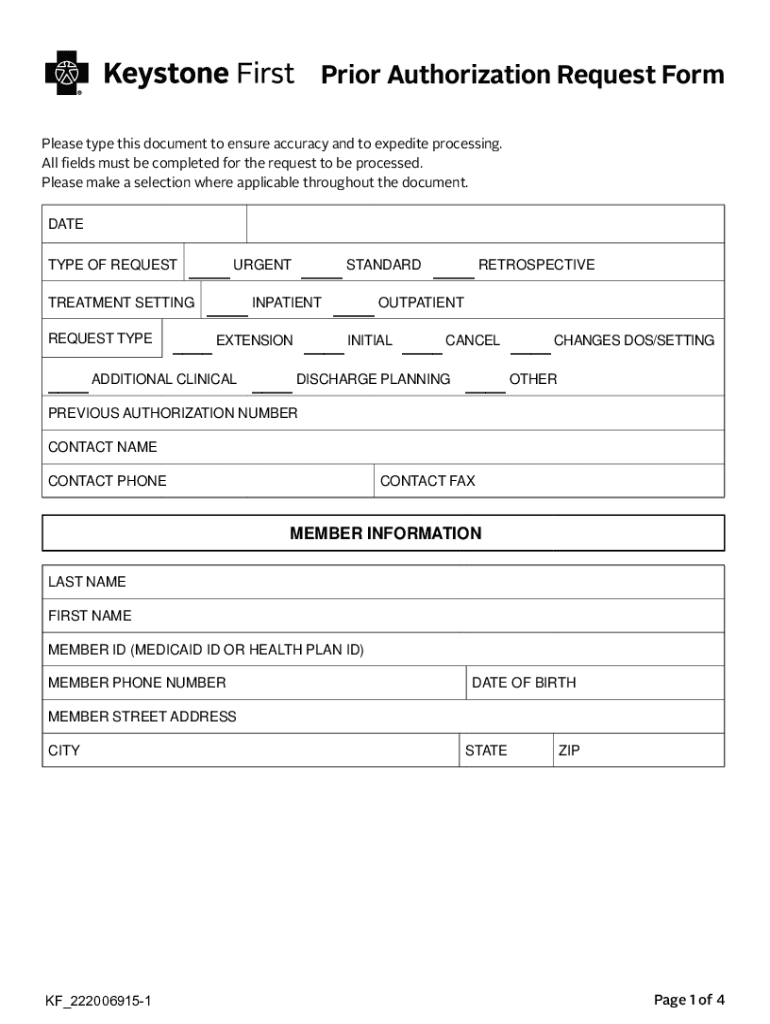
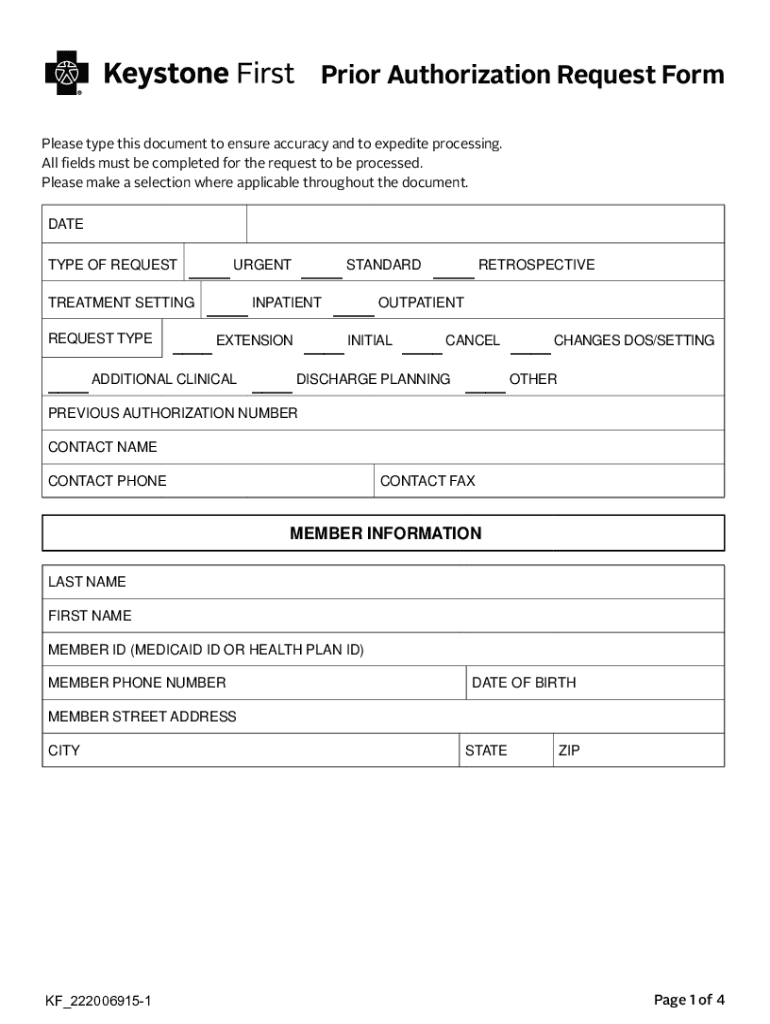
Before filling out a prior authorization request form, gathering correct and comprehensive information is vital. Start by assembling the necessary patient details, including their full name, date of birth, and insurance information. This information is foundational for the authorization request.
You also need provider information such as the name, contact details, and specialty of the healthcare professional requesting the service. Furthermore, provide specific details about the treatment, including the name of the medication, tests, or procedures involved in the request. Familiarizing yourself with your insurance guidelines is equally important; different insurers have varying requirements for what necessitates prior authorization. Ensuring you know which services require authorization can prevent unnecessary delays.
Step-by-step guide to completing the prior authorization request form
To initiate the prior authorization process, you first need to access the correct form designated by your insurer. This form is typically available on the provider's website or through their customer service. Downloading or printing the form will allow you to fill it out with the required information.
When filling out the prior authorization request form, ensure you complete each section thoroughly. Start with patient information, followed by provider details. For the requested services, provide detailed explanations and include any documentation required to support your request. Common mistakes include overlooking essential fields or submitting incomplete or inaccurate information, which can lead to delays or denials.
Submitting the prior authorization request
Submitting a prior authorization request can be done through several methods. Online portals, fax, and mail are popular options. Online submission is often the most efficient; however, it is crucial to weigh the pros and cons of each method. After submission, keeping a record of your request ensures you can track its progress.
Tracking your submission is essential for ensuring it is received and processed in a timely manner. Most insurers provide a confirmation process, allowing you to verify that your request has been logged. Familiarizing yourself with typical response timelines can help manage expectations and plan further steps in the treatment process.
What to expect after submission
After your prior authorization request has been submitted, it enters the review process conducted by the insurance company. During this phase, requests are evaluated for medical necessity. Insurers will look into whether the proposed treatment aligns with established guidelines, so presenting clear evidence of need is critical.
Responses from insurers will typically fall into two categories: approval and denial. An approval notification indicates that the insurer agrees to cover the requested service as medically necessary. On the other hand, if a denial occurs, understanding the reasons outlined by the insurer is vital, as it informs your options for appealing the decision.
Handling denials: steps for an effective appeal
Receiving a denial can be frustrating; however, knowing how to effectively appeal the decision can change the outcome. Understanding denial codes is the first step — these codes typically explain the insurer's reasoning behind the decision. This helps to identify any specific aspects that need addressing in your appeal.
Gathering supporting documentation is essential in bolstering your appeal. This could include medical records, letters from providers, or additional test results that support the necessity of the treatment. When preparing to file an appeal, follow the necessary procedures, and communicate clearly with providers and the insurer. Effective communication can significantly improve your chances of overturning a denial.
Utilizing technology for document management
Technological tools can enhance the prior authorization process significantly, particularly through platforms like pdfFiller. This cloud-based solution allows users to create and edit prior authorization request forms online, streamlining the submission process. The ease of accessing and managing documents in the cloud ensures that users can collaborate efficiently.
Among the numerous features of pdfFiller is the ability to eSign documents, providing a seamless way for all parties involved to consent to the authorization request. Moreover, the sharing capabilities allow relevant stakeholders to review and provide necessary input, thus enhancing communication and facilitating smoother documentation.
Best practices for managing prior authorization requests
Tracking prior authorization requests is vital for ensuring no steps are overlooked, which can lead to unnecessary delays in patient care. Maintaining a log of all submitted requests, including dates and outcomes, helps monitor the status of each authorization and identify any patterns in approvals or denials.
Additionally, ongoing communication with healthcare providers is important. Keeping providers informed about the status of authorizations can prevent disruptions in care and ensure that the necessary steps are being taken in a timely manner.
Real-world examples and case studies
Implementing effective prior authorization processes can lead to successful outcomes for both patients and providers. There are numerous success stories where clear communication and thorough documentation have resulted in timely approvals. For instance, a patient requiring a specific medication received approval within days because the provider submitted comprehensive documentation demonstrating its medical necessity.
Conversely, common pitfalls exist in the process, often resulting in long delays. Cases have shown that missing required information or failing to double-check the insurer's guidelines can result in denials. Learning from these experiences highlights the importance of meticulous attention to detail in each step of the prior authorization process.
Frequently asked questions (FAQs)
A variety of inquiries surround the topic of prior authorization, ranging from general questions about the necessity of the process to specific queries regarding the completion of the request form. Understanding how to appropriately handle scenarios like urgent requests or unusual cases can ease the journey through the prior authorization process.
Developing a clear understanding of the prior authorization request form is essential for anyone involved in the healthcare process, ensuring that patients receive their necessary treatments promptly and efficiently. Whether a healthcare provider, patient, or administrative staff, grasping the nuances of this process can make all the difference in healthcare outcomes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my prior authorization request form directly from Gmail?
How can I modify prior authorization request form without leaving Google Drive?
How do I complete prior authorization request form online?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.