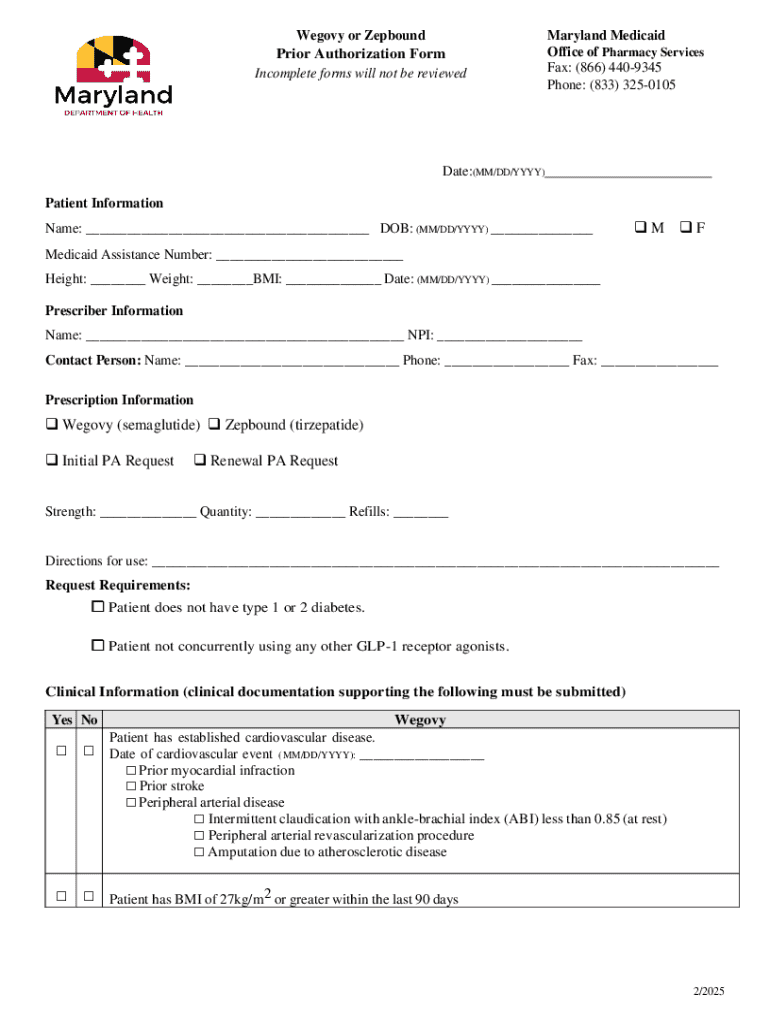
Get the free wegovy prior authorization form
Get, Create, Make and Sign wegovy prior authorization form



How to edit wegovy prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out wegovy prior authorization form

How to fill out wegovy or zepbound prior
Who needs wegovy or zepbound prior?
Wegovy or Zepbound prior form: a comprehensive guide
Understanding Wegovy and Zepbound
Wegovy and Zepbound are two medications gaining attention for their roles in weight management and metabolic health. Wegovy, a brand name for semaglutide, is an injectable prescription medication specifically developed for chronic weight management. Clinical studies have shown it can significantly reduce body weight alongside diet and exercise, making it a valuable tool for individuals struggling with obesity. On the other hand, Zepbound, also known as tirzepatide, is a newer medication currently under review and is designed for metabolic conditions, including obesity and type 2 diabetes.
Both medications work by mimicking hormones that target the areas of the brain regulating hunger and satiety. This unique mechanism helps individuals achieve better control over their eating habits and improves overall health outcomes. Understanding these drugs is essential, especially in light of healthcare policies surrounding their prescriptions.
The importance of prior authorizations in healthcare
Prior authorizations are crucial steps in the healthcare system, particularly regarding expensive medications like Wegovy and Zepbound. A prior authorization refers to the process whereby a healthcare provider must obtain approval from a patient's insurance before commencing treatment. This process ensures that treatments are medically necessary and that the insurance provider will cover the associated costs.
The importance of prior authorizations cannot be overstated, especially in today’s constantly evolving healthcare landscape. They help control costs, manage patient access to medications, and ensure that specific patient criteria are met. For Wegovy and Zepbound, obtaining a prior authorization can often feel like a necessary hurdle, but it’s essential for guaranteeing that these medications are used appropriately.
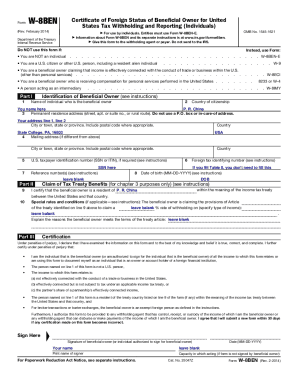
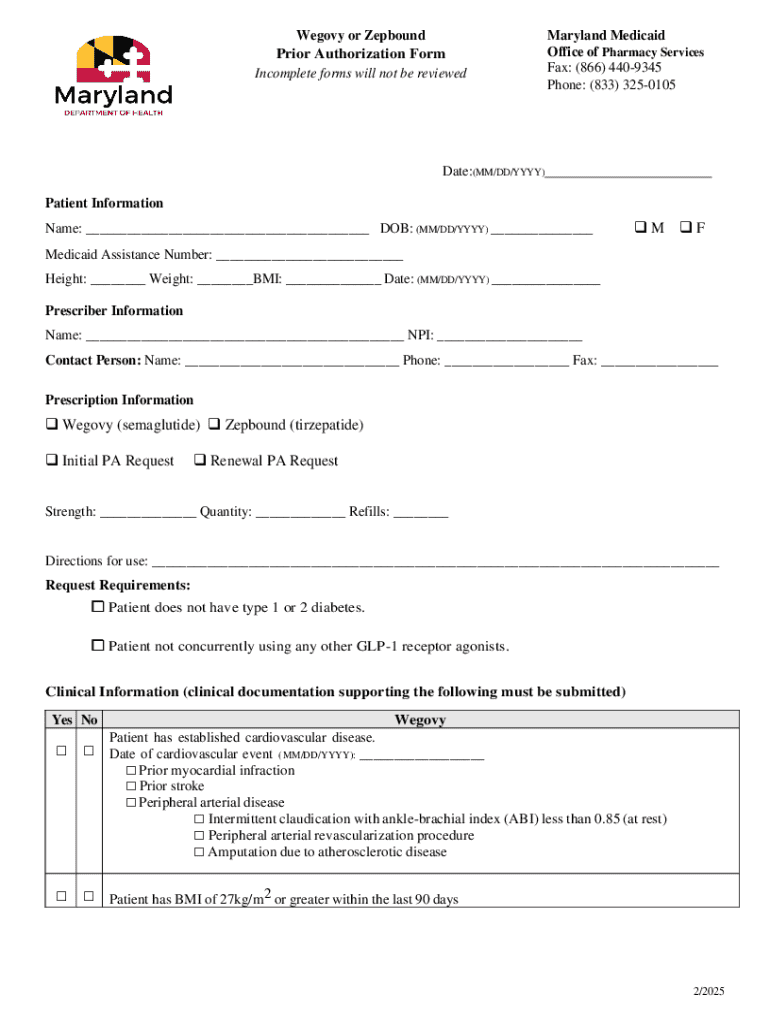
The prior authorization process for Wegovy and Zepbound
Navigating the prior authorization process for Wegovy and Zepbound requires careful attention to detail and a thorough understanding of the necessary documentation. Here are the essential steps to take when initiating a prior authorization:
After gathering the necessary documentation and completing the form, submission procedures vary, with electronic channels generally preferred for their speed and efficiency. Timelines for reviews can differ based on the insurance provider, but knowing your estimated wait time can help you manage patient expectations.
Common information required for prior authorization
When seeking a prior authorization for Wegovy and Zepbound, specific information is crucial. A detailed documentation checklist is essential to ensure that nothing is overlooked. Key elements that should be included are:
Indications for approval often hinge on medical necessity criteria. It's essential that healthcare providers understand the specific criteria established by insurers for both Wegovy and Zepbound to ensure the best chance of approval.
The role of technology in managing prior authorizations
With the rise in digital healthcare management tools and platforms, managing prior authorizations has become more streamlined. Utilizing cloud-based platforms, such as pdfFiller, enhances the process dramatically through various features that simplify submissions. For example, pdfFiller allows users to edit documents easily, sign electronically, and collaborate seamlessly with healthcare teams.
This technological advancement not only speeds up the prior authorization process but also helps eliminate common issues such as lost documents and mishandled submissions. Cloud-based platforms also support remote access capabilities, making it easier for healthcare teams to handle submissions from anywhere.
Challenges in obtaining prior authorization for Wegovy and Zepbound
While the process of obtaining a prior authorization is critical, it is not without challenges. Common hurdles include differences in insurance policies, which can vary widely from one plan to another, often leading to confusion. Incomplete submissions frequently cause delays, resulting in additional frustration for patients and healthcare providers alike.
To overcome these challenges, consider implementing the following strategies:
Using a systematic approach to prior authorizations will minimize setbacks and enhance the overall efficiency of the process.
Frequently asked questions (FAQs) about Wegovy and Zepbound prior forms
Understanding the nuances of prior authorization can raise several questions for patients and healthcare providers alike. Here are some frequently asked questions relevant to Wegovy and Zepbound:
Best practices for filling out prior authorization forms
Successfully completing a prior authorization form for Wegovy or Zepbound requires careful attention to detail. Here are some best practices to ensure your submission is accurate:
Additionally, aiming for quick turnaround should be a priority. Organizing your files and using technology such as pdfFiller helps speed up the submission process and keep everything on track.
Leveraging pdfFiller in your workflow
pdfFiller serves as a powerful tool for managing your prior authorization needs. Users can experience seamless document editing and management, enabling them to craft well-structured submissions even on-the-go. The platform’s remote access capabilities empower healthcare teams to maintain productivity whether in the office or working remotely.
A plethora of case studies reveal the significant improvements in workflows for healthcare providers utilizing pdfFiller to manage prior authorizations. Testimonials highlight how this tool has led to faster approvals and improved patient outcomes.
Additional tools and resources
Enhancing your understanding of the prior authorization process is essential. Numerous resources are available to assist users with specific issues related to Wegovy and Zepbound prior forms. Look for step-by-step video guides that demonstrate filling out forms effectively while also accessing templates that help outline medical necessity.
If you encounter further inquiries, pdfFiller support is accessible for any document-related questions. Additionally, reaching out to your insurance provider for personalized assistance can provide clarity throughout the authorization process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I execute wegovy prior authorization form online?
How do I make edits in wegovy prior authorization form without leaving Chrome?
How can I edit wegovy prior authorization form on a smartphone?
What is wegovy or zepbound prior?
Who is required to file wegovy or zepbound prior?
How to fill out wegovy or zepbound prior?
What is the purpose of wegovy or zepbound prior?
What information must be reported on wegovy or zepbound prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.