Stroke orientation checklist for form
Understanding stroke orientation checklists
A stroke orientation checklist is a structured tool designed to guide healthcare professionals in providing comprehensive care to stroke patients. The primary purpose of this checklist is to ensure that all key aspects of patient assessment, education, and follow-up care are thoroughly addressed. This systematic approach to managing stroke care enhances patient outcomes by promoting timely intervention and effective recovery strategies.
The importance of stroke orientation in patient care cannot be overstated. Stroke is a leading cause of long-term disability and can significantly impact a patient's quality of life. By utilizing a checklist, healthcare providers can ensure that they do not overlook critical elements during patient evaluation and treatment processes. This leads to optimized care, better patient understanding, and ultimately, improved rehabilitation and recovery.
Key components of a stroke orientation checklist
An effective stroke orientation checklist encompasses multiple components that facilitate holistic patient care. At its core, the checklist should include assessment criteria, educational materials, and resources for post-stroke support.
This includes a thorough neurological evaluation and the use of standardized physical assessment tools to gauge the patient's condition.
Developing informational pamphlets, videos, and interactive content helps equip patients with vital knowledge about their condition and recovery.
These may include scheduling follow-up appointments and access to referral services, ensuring continuous care post-discharge.
Creating an effective stroke orientation checklist
Designing a stroke orientation checklist requires careful consideration and collaboration. Here’s a step-by-step guide to developing a comprehensive checklist tailored to your patient population.
Understand the demographics and specific challenges faced by your patient population to create a customized checklist.
Consult with neurologists, nurses, therapists, and other professionals to ensure the checklist covers all necessary aspects.
Utilize guidelines and recommendations from recognized stroke care organizations to align your checklist with best practices.
Formatting is essential for usability. Ensure that the checklist is well-organized for easy navigation, using clear headings and sections to guide users. Including visuals and diagrams can enhance understanding and retention of information.
Using the stroke orientation checklist effectively
To maximize the benefits of a stroke orientation checklist, effective training for healthcare providers is crucial. Workshops and seminars can provide hands-on training on how to utilize the checklist in various clinical settings.
In-person training sessions that enable staff to understand the checklist and its application in patient care.
Utilize digital platforms to offer training modules that can be accessed anywhere, facilitating ongoing education.
Application scenarios for the checklist include inpatient care settings where immediate assessment is critical, and outpatient rehabilitation where consistent follow-up is necessary to track recovery progress.
Integrating technology into stroke orientation checklists
The incorporation of technology can significantly enhance the accessibility and effectiveness of stroke orientation checklists. Digital tools allow for simpler management and real-time updates, improving the user experience for healthcare providers and patients alike.
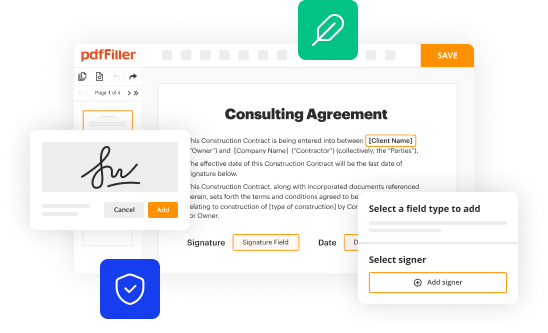
Develop apps where healthcare professionals can quickly access and complete checklists digitally during patient encounters.
Enable secure storage and sharing of checklists across teams, ensuring that all providers have the most current information.
Additionally, integrating interactive features such as real-time feedback mechanisms and gamification elements can enhance patient engagement. This approach makes learning about stroke recovery more interactive and less daunting.
Best practices for implementing the stroke orientation checklist
Successful implementation of a stroke orientation checklist lies in collaboration among healthcare teams. Clearly defined roles and responsibilities help ensure that every team member understands their contribution to patient care.
Clarify who is responsible for which aspects of patient care and checklist completion to streamline processes.
Utilize consistent communication methods among team members to share important updates and feedback regarding patient progress.
Additionally, a continuous improvement process should be in place. Regularly soliciting feedback from patients and staff can provide valuable insights for updates and refinements to the checklist, ensuring it remains effective and relevant.
Case studies and success stories
Examining real-world examples can provide evidence of the effectiveness of stroke orientation checklists. Successful implementations have demonstrated significant improvements in patient outcomes and increased staff efficiency.
Hospitals that adopted standardized checklists saw a notable reduction in complications and shorter recovery times.
Healthcare professionals have reported increased confidence in managing stroke patients using checklists following improved training and resources.
These success stories highlight the value of developing a comprehensive stroke orientation checklist, reinforcing its foundational role in enhancing care delivery.
Evaluating the effectiveness of stroke orientation checklists
To determine the success of a stroke orientation checklist, it's essential to establish metrics that evaluate its effectiveness. Key performance indicators include measuring patient understanding and retention of information as well as monitoring reductions in hospital readmissions.
Evaluate how well patients comprehend and remember the information provided through the checklist.
Track statistics related to readmission rates to assess the impact of the checklist on long-term patient outcomes.
Ongoing research in stroke management continues to uncover emerging trends and innovations. Staying informed about these developments will further enhance the effectiveness of stroke orientation checklists.
Contacting specialized help and resources
Networking with stroke care experts and local resources can provide additional support for healthcare providers and patients alike. Accessing specialized rehabilitation facilities and contacting local stroke services ensures that patients receive the utmost care tailored to their needs.
Establish connections with organizations that focus on stroke support to facilitate patient referrals.
Encourage the formation of community support groups that can offer vital peer support to stroke survivors and families.
Utilizing these networks can significantly enhance patient recovery and quality of life.
Conclusion on stroke orientation data management
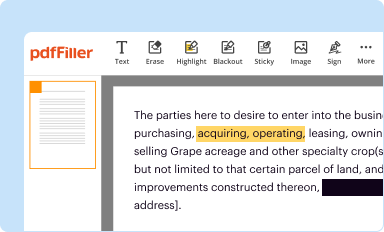
The importance of using digital solutions, such as those offered by pdfFiller, cannot be overstated in managing stroke orientation checklists. These tools empower users to manage their checklists with efficiency and ease.
Users can easily edit checklist forms and update patient information without hassle.
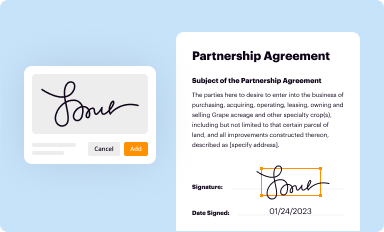
These functionalities allow for straightforward approvals and shared access to the checklist, fostering teamwork in patient care.
Ultimately, adopting effective stroke orientation checklists coupled with advanced document management solutions can significantly enhance patient care, promote better outcomes, and streamline communication among healthcare providers.