
Get the free Wegovy Drug Prior Authorization Form
Get, Create, Make and Sign wegovy drug prior authorization
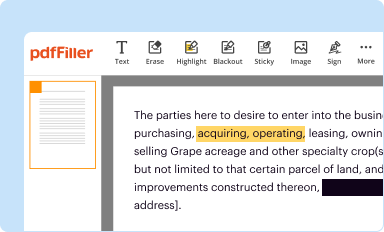
Editing wegovy drug prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out wegovy drug prior authorization
How to fill out wegovy drug prior authorization
Who needs wegovy drug prior authorization?
Wegovy Drug Prior Authorization Form: A Comprehensive How-to Guide
Understanding prior authorization for Wegovy
Prior authorization is a process used by health insurance companies to determine the medical necessity of a prescribed medication before approving payment. This protocol is critical in ensuring that the medication approach is the most effective way to address a patient's condition. For Wegovy, a weight management drug that contains semaglutide, prior authorization is especially significant. It not only guarantees coverage for the patient but also aligns treatment with clinical guidelines.
Wegovy is specifically designed to aid in chronic weight management, complementing a reduced-calorie diet and increased physical activity. It is indicated for adults with a body mass index (BMI) of 30 or greater or 27 or greater with at least one weight-related medical condition. Understanding the importance of prior authorization is key, as it can significantly affect your journey toward effective weight management.
Who needs to complete the Wegovy prior authorization form?
Patients who are prescribed Wegovy by their healthcare providers typically need to comply with the prior authorization process. Eligibility includes having a valid diagnosis that warrants the use of Wegovy and ensuring that previous weight loss attempts have been documented. It is also essential for healthcare providers to be aware of their patient's insurance policies and the associated requirements for prior authorization.
Overview of the Wegovy prior authorization form
The Wegovy prior authorization form requires comprehensive patient and provider information. It typically includes sections for patient demographics, medication details, medical and treatment history, and supporting clinical documentation. Providing accurate and complete information in these sections is vital for a swift review process.
Step-by-step instructions for filling out the Wegovy prior authorization form
Filling out the Wegovy prior authorization form involves meticulous attention to detail. First, prepare all necessary documentation, which includes the patient's medical history, outcomes from previous weight-loss attempts, and any relevant clinical evidence endorsing the use of Wegovy. This thorough preparatory step can simplify the filling process.
Each section of the form requires particular attention. Ensure that you gather detailed information about the patient, the prescribed medication (including dosing details), the provider's contact information, and a well-crafted clinical justification for why Wegovy is necessary.
Submitting the Wegovy prior authorization form
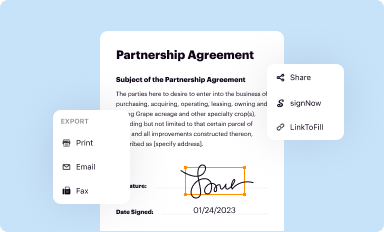
Once completed, the Wegovy prior authorization form can be submitted through various methods. Most commonly, it can be sent online or via traditional fax. Each method has unique specifics, so ensure you follow what your insurance provider requires for effective processing.
After submission, it’s important to follow up. Knowing who to contact and understanding the timeline for response can help you address any potential delays or gather further information if needed.
Managing responses to your prior authorization request
Receiving a response to your prior authorization request for Wegovy can lead to two outcomes: approval or denial. Understanding the implications of each response is crucial. If approved, the patient can proceed with acquiring Wegovy. If denied, it’s essential to have a plan in place to manage the situation.
Denials can stem from various factors, including incompletion of the form, lack of medical necessity, or failure to meet specific insurance criteria. Being prepared with an appeals process can aid in securing medication access despite initial setbacks.
Utilizing pdfFiller for your prior authorization needs
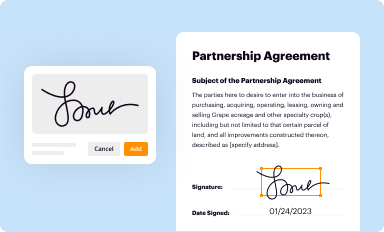
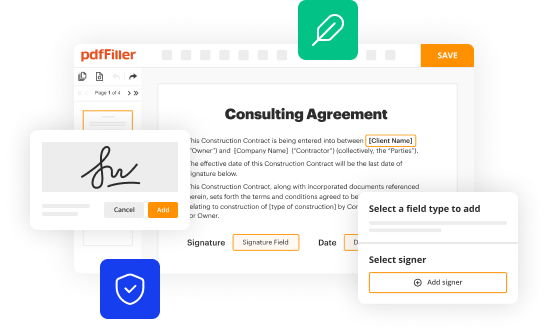
Managing the Wegovy prior authorization form can be streamlined using pdfFiller. This platform empowers users by enabling easy editing, signing, and document management in a cloud-based environment. It ensures you can access your filled forms anywhere, anytime.
pdfFiller's features let you seamlessly collaborate with team members or healthcare providers, simplifying the entire prior authorization process.
Avoiding common mistakes in the prior authorization process
Errors during the prior authorization process can lead to delays or denials. Common mistakes include incomplete forms, inaccurate patient or provider details, and insufficient clinical justification for the medication. To ensure a successful submission, it can be beneficial to follow a checklist.
Attention to detail is paramount. By avoiding common pitfalls and adhering to best practices, you can increase the likelihood of your authorization request being approved.
Enhancing your understanding of Wegovy and related treatments
To maximize the efficacy of treating weight-related conditions with Wegovy, it's beneficial to stay informed about additional resources and treatment options. Professional organizations often provide materials that can enhance understanding and offer support for patients and healthcare practitioners alike.
Support groups and hotlines available can help individuals experiencing challenges related to weight management. Keeping up with the latest research into Wegovy and similar treatments enables patients and providers to make informed decisions.
Staying updated on prior authorization changes
Healthcare policies and insurance criteria are constantly evolving, impacting prior authorization processes, including those for Wegovy. It’s crucial for both patients and providers to stay informed about any changes that could affect authorization eligibility and requirements.
Regular communication with insurance providers and monitoring updates will ensure compliance with current criteria, improving the chances of successful authorization.
Interactive tools for prior authorization management
pdfFiller's interactive tools play a significant role in managing the Wegovy prior authorization process. These tools allow for synchronous collaboration, ensuring that all involved parties can contribute to the documentation without any communication barriers.
By facilitating comprehensive document sharing and management solutions, pdfFiller enhances user experience and ensures that form submissions are as smooth and error-free as possible.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my wegovy drug prior authorization in Gmail?
How can I get wegovy drug prior authorization?
How do I fill out the wegovy drug prior authorization form on my smartphone?
What is wegovy drug prior authorization?
Who is required to file wegovy drug prior authorization?
How to fill out wegovy drug prior authorization?
What is the purpose of wegovy drug prior authorization?
What information must be reported on wegovy drug prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.






















