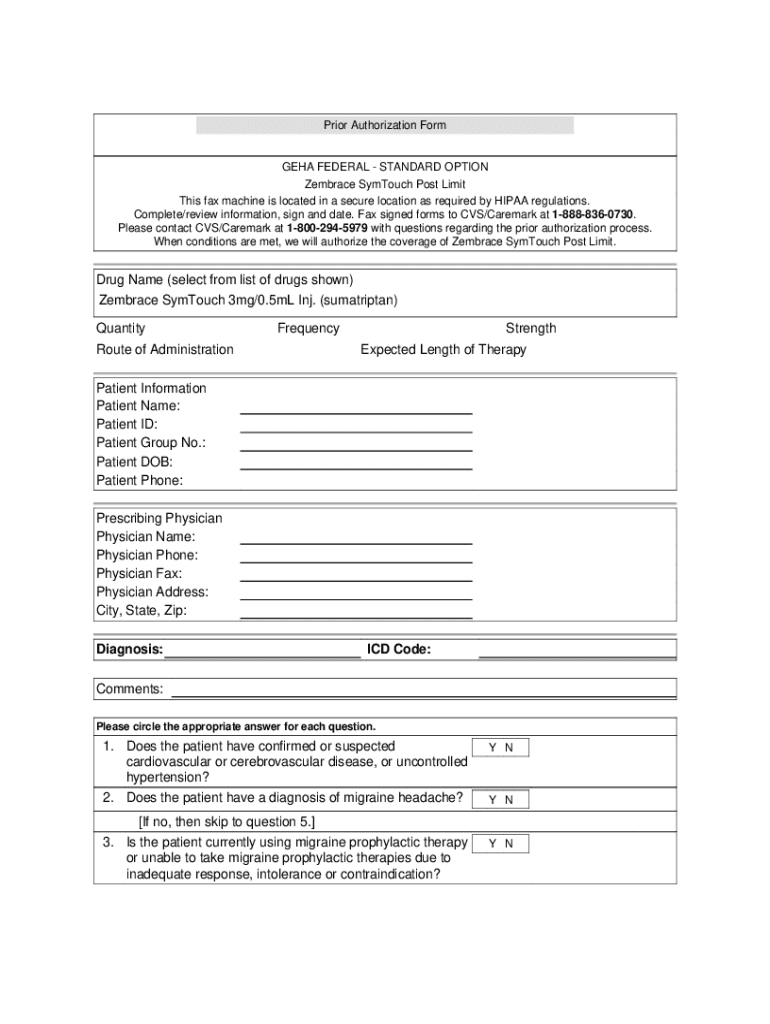
Get the free geha prior authorization general form
Get, Create, Make and Sign geha prior authorization form pdf



Editing geha prior authorization general online
Uncompromising security for your PDF editing and eSignature needs
How to fill out geha prior authorization general

How to fill out prior authorization form
Who needs prior authorization form?
A Comprehensive Guide to Prior Authorization Forms
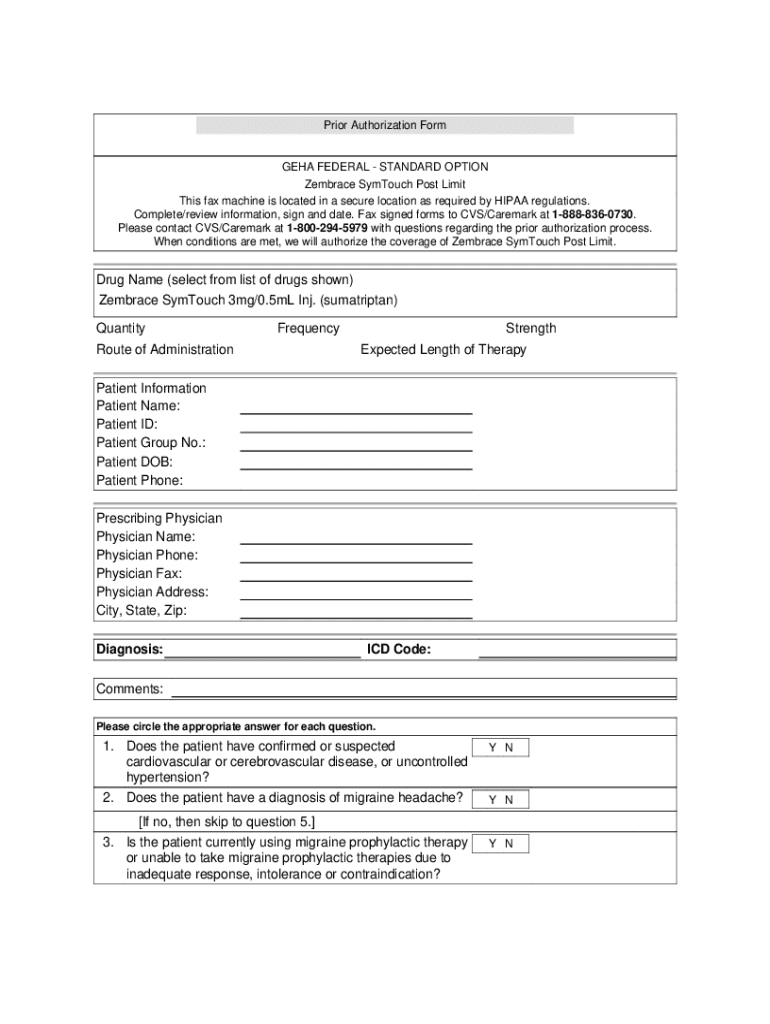
Understanding prior authorization forms
Prior authorization forms are essential documents in the healthcare system that require approval from an insurance company before a specific service or medication is provided to patients. This process ensures that the proposed treatment aligns with the patient’s medical necessity and the insurance coverage guidelines.
The importance of prior authorization cannot be overstated; it safeguards against unnecessary treatments, helps manage healthcare costs, and ensures that patients receive appropriate care. Both patients and healthcare providers face challenges during this process, and understanding the prerequisites can smooth the path to timely care.
Types of prior authorization forms
Different types of prior authorization forms cater to an array of medical services. The most common categories include those for specialty medications, imaging services like MRIs and CT scans, surgical procedures, mental health treatments, and instances of emergency care.
Key components of a prior authorization form
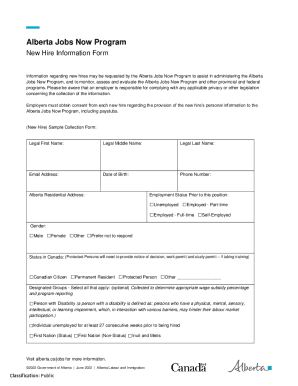
Completing a prior authorization form requires a thorough filling of information to facilitate smooth processing. Key components include patient information, provider details, insurance policy specifics, the requested service description, and required supporting documentation.
Steps to fill out a prior authorization form
Filling out a prior authorization form may seem daunting, but following clear steps can streamline the process. To begin, gather all necessary information regarding the patient's medical history and specific insurance policy details.
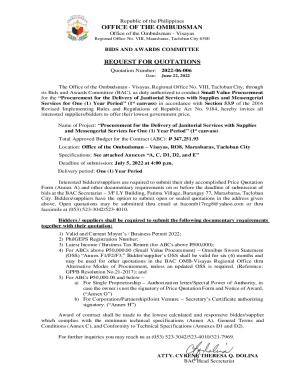
Submitting the prior authorization form
Once completed, the prior authorization form must be submitted. There are two primary methods of submission: paper and electronic. Electronic submission is typically preferred; however, understanding the protocols for both is crucial.
Tracking the status of your prior authorization
After submission, tracking the status of a prior authorization request is vital to ensure approvals are timely. Generally, approvals can take several days to weeks depending on the insurance provider and the complexity of the request.
Managing your prior authorization documents
Thorough management of prior authorization documents is essential not only for efficiency but also for compliance with regulations. Using a platform like pdfFiller can greatly simplify this task, as it offers tools for storing, organizing, and collaborating on these essential documents.
Tips for a successful prior authorization experience
Navigating prior authorization can be complicated, but effective communication and careful documentation can significantly ease the experience. Keeping in close contact with your healthcare provider ensures all necessary information is conveyed.
Additional features of pdfFiller for prior authorization forms
One of the standout features of pdfFiller is its interactive tools that enhance the prior authorization process. By offering cloud-based access, users can conveniently fill out forms, edit documents, and collaborate with their teams regardless of their location.
Frequently asked questions (FAQs) about prior authorization forms
Understanding the nuances of prior authorization forms can lead to several questions. Addressing these FAQs helps in demystifying the process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit geha prior authorization general from Google Drive?
How do I make edits in geha prior authorization general without leaving Chrome?
How can I edit geha prior authorization general on a smartphone?
What is prior authorization form?
Who is required to file prior authorization form?
How to fill out prior authorization form?
What is the purpose of prior authorization form?
What information must be reported on prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.