
Get the free Prior Authorization Request Form
Get, Create, Make and Sign prior authorization request form
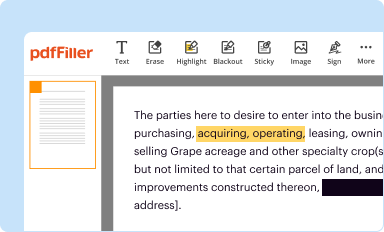
Editing prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form
How to fill out prior authorization request form
Who needs prior authorization request form?
Understanding and Navigating the Prior Authorization Request Form
Understanding prior authorization
Prior authorization is a process used by health insurance companies to determine if a service, treatment, or medication is medically necessary before they agree to pay for it. This preemptive step helps insurers manage costs and ensure that patients receive appropriate care based on established medical guidelines.
The importance of prior authorization in healthcare cannot be overstated. It not only safeguards patients from unnecessary treatments but also curbs expenses incurred by insurers. Various scenarios may trigger the need for prior authorization, such as costly medications, specialized procedures, or non-standard treatments that significantly deviate from established care protocols.
Key components of a prior authorization request form
A prior authorization request form is structured to gather specific information critical to the review process. The components can be categorized as follows:
Step-by-step guide to filling out a prior authorization request form
Completing a prior authorization request form accurately is crucial to ensure timely approvals. Begin by gathering all necessary information.
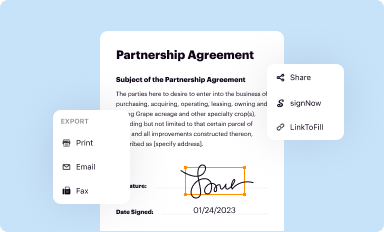
Submitting your prior authorization request
Once the form is filled out, the next step involves submitting it to the insurance company. Today's digital landscape allows for multiple submission methods, ensuring flexibility.
Responding to prior authorization decisions
Once submitted, the insurance company will review your request and convey approval or denial notifications. Understanding these notifications is vital.
Common challenges with prior authorization
Navigating the prior authorization landscape can present several challenges. Delays in approvals can significantly affect patient care, leading to unnecessary wait times and treatment interruptions.
Resources for further assistance
Having access to adequate resources can provide additional support when dealing with prior authorization processes. Knowing where to turn for help can change the game.
Utilizing pdfFiller for your prior authorization requests
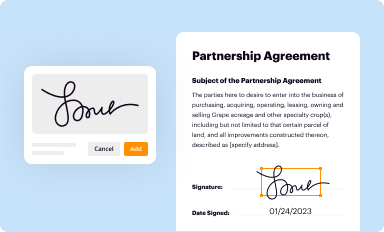
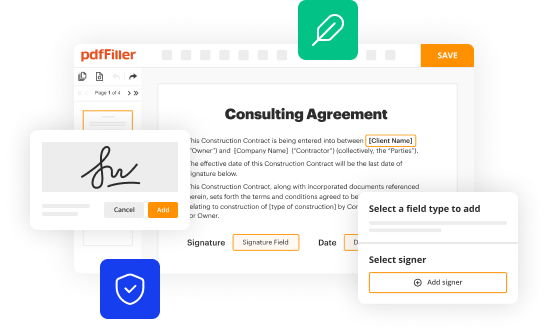
pdfFiller offers a streamlined approach to managing your prior authorization documents. Its user-friendly features enable users to edit, sign, and collaborate on forms from any location.
Appendix
For quick reference and assistance, the appendix contains a sample prior authorization request form, frequently asked questions about prior authorization, and a glossary of relevant terms.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my prior authorization request form in Gmail?
Can I edit prior authorization request form on an iOS device?
How do I complete prior authorization request form on an iOS device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.






















