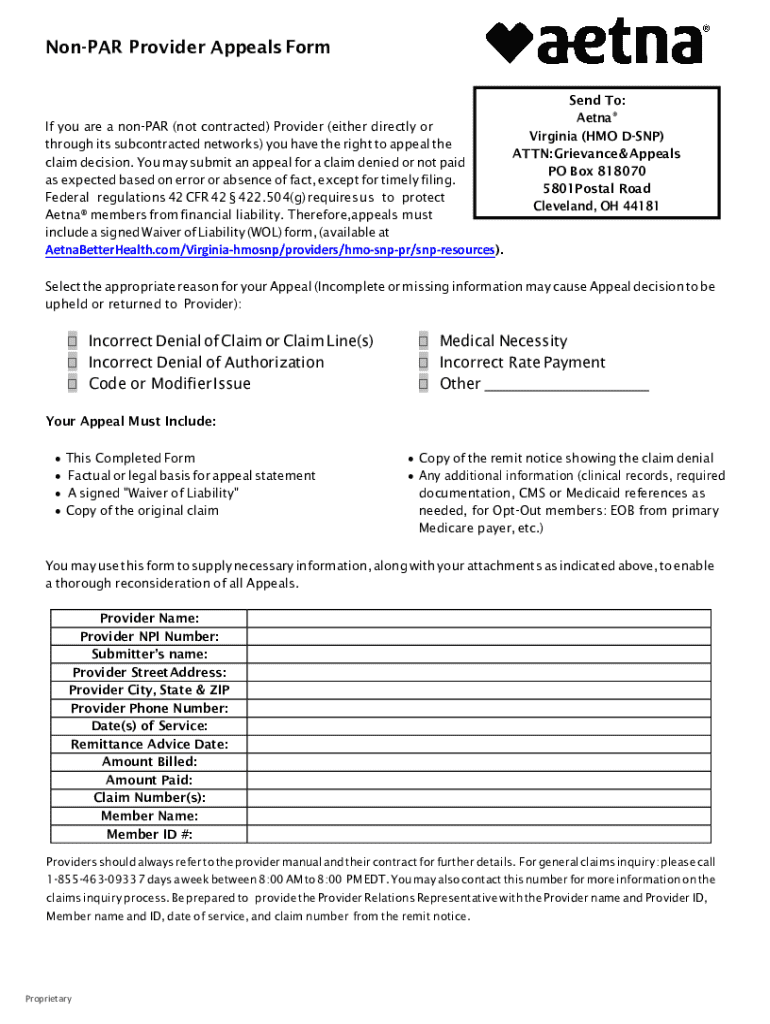
Get the free Non-par Provider Appealsform
Get, Create, Make and Sign non-par provider appealsform
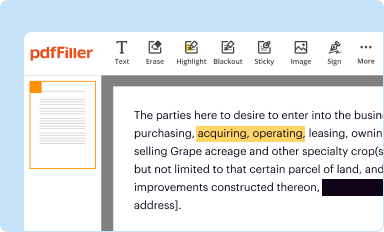
How to edit non-par provider appealsform online
Uncompromising security for your PDF editing and eSignature needs
How to fill out non-par provider appealsform
How to fill out non-par provider appealsform
Who needs non-par provider appealsform?
Navigating the Non-Par Provider Appeals Form: A Comprehensive Guide
Understanding non-par provider appeals
A non-participating provider, or non-par provider, is a healthcare professional or facility that does not have a contract with a health insurance plan. Unlike participating providers who have agreed to accept specific payment rates from insurers, non-par providers typically charge patients their full rates, leading to potential out-of-pocket expenses. Patients may opt for non-par providers for various reasons, including a lack of available participating providers or preferred treatment options.
Appeals play a critical role in healthcare, particularly when accessing necessary services. Patients often face challenges with insurance decisions that deny coverage for specific medical treatments or services provided by non-par providers. Common reasons for appeals include incorrect billing, lack of pre-authorization, or disagreement with treatment necessity. Understanding the appeals process is essential for maximizing the chances of securing coverage.
The non-par provider appeals process
The appeals process generally involves several key steps that patients need to follow diligently. Firstly, once a denial is received, the patient should review the explanation provided by the insurer. This often includes specific codes or reasons for denial. The next step is to gather relevant information, including medical records, bills, and any other supporting documentation. Timely submission of the appeal is also crucial, as many insurers have strict deadlines—usually between 30 to 180 days post-denial.
Filling out the non-par provider appeals form
Completing the non-par provider appeals form can significantly impact the outcome of your appeal. The form typically consists of sections that request patient information, provider details, insurance policy numbers, and specific reasons for the appeal. It's essential to ensure that all fields are filled accurately to avoid delays.
Common mistakes when filling out the form include incorrect personal information, failing to provide adequate detail regarding the treatment or service contested, and not including relevant documentation. To prevent these issues, double-check the completed form before submission and consider having someone else review it for clarity and completeness.
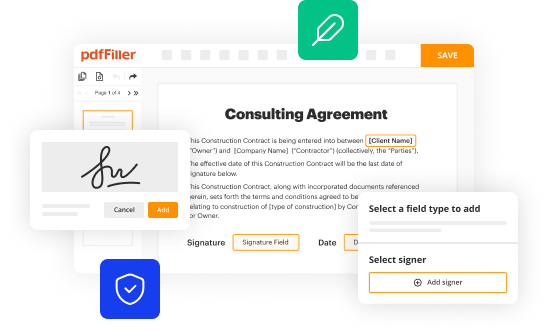
Utilizing tools like pdfFiller can facilitate the form-filling process, allowing users to edit, sign, and complete the document online. This makes it easier to manage your appeal efficiently.
Submitting your appeal: best practices
The manner in which you submit your appeal can also influence its timely processing. Most insurers provide options for electronic submissions via their websites or portals, which are generally faster than traditional mail. Ensure that you keep records of everything submitted, including confirmation numbers if applicable.
After submitting your appeal, it's wise to follow up with the insurance provider. This ensures that they have received your documents and that the processing is underway. Document any follow-up communications as they could be crucial if further action is needed.
Understanding your rights in the appeals process
As a patient, understanding your rights during the appeals process is paramount. You have the right to appeal any denial made by your insurer concerning necessary medical services, including those involving non-par providers. Federal laws, such as the Employee Retirement Income Security Act (ERISA), as well as various state laws, establish guidelines for fair handling of appeals.
In cases where an appeal is denied, there are resources available for further actions, such as contacting patient advocacy organizations that can assist in navigating the next steps.
What happens after you submit your appeal?
Once your appeal is submitted, it typically enters a review process that can vary in duration. Insurers are usually mandated to complete their reviews within a specific timeframe, often 30 to 60 days. During this period, they may reach out for additional information or clarification.
Preparation for potential next steps is vital, especially if the insurer denies your appeal. Understanding the reason for the denial can aid in formulating a subsequent appeal or alternative actions.
Tips for successfully navigating the appeals process
Navigating the appeals process effectively requires persistence and a well-organized approach. Personalizing your appeal with specific case details and narratives can enhance its impact. Organizing your documentation and maintaining clear communication with your insurer can significantly improve your chances of a favorable outcome.
In certain cases, seeking help from professionals, such as healthcare advocates or legal counsel, may prove beneficial. They can provide guidance on how to handle complex cases and ensure that your rights are protected.
Leveraging pdfFiller for your appeal needs
Using pdfFiller can streamline the entire appeals process. With its robust features, users are empowered to edit, sign, and manage documents all in one place, enhancing efficiency. The intuitive user interface allows for seamless form completion, reducing the likelihood of errors and improving clarity.
Success stories abound for individuals who have utilized pdfFiller while navigating their appeals. Many report that having a centralized platform for document management not only relieved stress but also improved their communication and organization.
FAQs about non-par provider appeals forms
With appeals being a crucial aspect of healthcare, many individuals have similar concerns. Common questions circulate around timelines, types of information required in appeals, and procedures following a denial. Clarifying these terms and conditions helps alleviate confusion.
Understanding these FAQs equips patients with the knowledge necessary to navigate the appeals process confidently, enabling them to secure the healthcare they need.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify non-par provider appealsform without leaving Google Drive?
How do I make edits in non-par provider appealsform without leaving Chrome?
How do I fill out non-par provider appealsform on an Android device?
What is non-par provider appeals form?
Who is required to file non-par provider appeals form?
How to fill out non-par provider appeals form?
What is the purpose of non-par provider appeals form?
What information must be reported on non-par provider appeals form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.