
Get the free Changes to Medical Necessity Review Criteria for Physical, Occupational, and Speech ...
Get, Create, Make and Sign changes to medical necessity
How to edit changes to medical necessity online
Uncompromising security for your PDF editing and eSignature needs
How to fill out changes to medical necessity
How to fill out changes to medical necessity
Who needs changes to medical necessity?
Changes to Medical Necessity Form: A Comprehensive Guide
Overview of medical necessity forms
Medical necessity forms are essential documents used in healthcare to justify the need for specific medical services or items. These forms ensure that treatments and equipment are necessary for the patient's health condition and compliance with insurance requirements. The primary purpose of these forms is to facilitate reimbursement from insurance companies by validating that the service provided meets defined medical guidelines. This documentation is crucial for securing payment for healthcare providers and ensuring patients receive the care they require.
The importance of medical necessity forms extends beyond reimbursement; they play a vital role in promoting patient safety and appropriate care. When healthcare providers complete these forms accurately, they establish a clear link between patient needs and the services rendered. This not only supports financial transactions but also helps prevent potential clinical disputes related to care decisions, ultimately fostering trust between providers and patients.
Key changes to medical necessity forms
Recent revisions in regulations surrounding medical necessity forms have brought significant changes to how these documents are structured and the information they require. The Centers for Medicare & Medicaid Services (CMS) have implemented new standards aimed at improving clarity and efficiency in the submission process. For instance, certain formats have been standardized across various healthcare settings to streamline documentation and minimize redundancy.
Among the specific changes to formats and content requirements are several new sections and fields. Healthcare providers may now notice the introduction of areas that necessitate additional clinical information or patient history, enhancing the justification process. Conversely, some previously required fields have been eliminated to simplify the form-filling experience. Understanding these modifications is crucial for healthcare providers, as compliance with updated forms can directly impact claims approval.
For healthcare providers, understanding these changes is paramount to avoid claims denials and ensure continual patient service delivery.
How changes affect patient care
The modifications to medical necessity forms can have a profound impact on patient care, primarily affecting access to necessary services. By introducing more comprehensive detail requirements within these forms, patients may experience delays if their healthcare providers do not complete the forms accurately or promptly. This can hinder timely access to crucial treatments and equipment, particularly for critical items like durable medical equipment (DME).
However, the updated forms also present an opportunity for enhanced patient advocacy. With clearer documentation expectations, healthcare providers can present a stronger case for necessary treatments, particularly in complex scenarios. The onus of ensuring compliance lies partly with healthcare providers, who must familiarize themselves with the latest regulations and adapt their practices accordingly.
Step-by-step guide to updating medical necessity forms
Updating medical necessity forms involves a systematic approach. First, healthcare providers should assess their current forms to identify gaps concerning the new requirements. A thorough review will help familiarize practitioners with both required and optional fields to avoid common mistakes that lead to claims rejection.
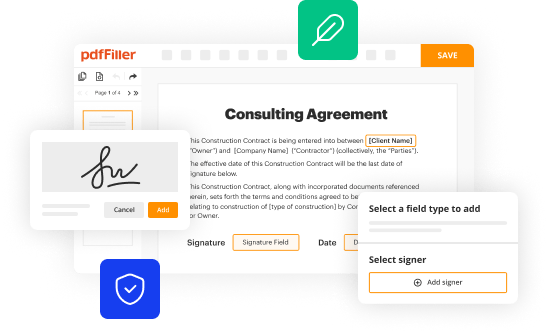
After assessing current forms, providers must incorporate the updated regulations into their processing procedures. This requires training staff on the new form structures and ensuring all operational workflows move in sync with these changes. Modern technologies, such as the pdfFiller platform, offer user-friendly ways to manage this transition efficiently.
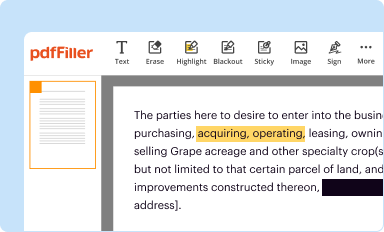
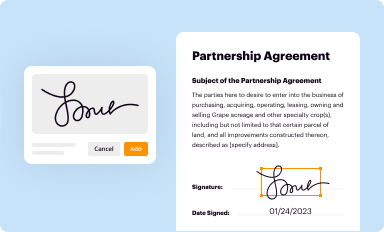
Using pdfFiller, providers can fill out and manage forms seamlessly. It offers tools that allow users to not only fill out forms but also edit existing ones, add eSignatures, and collaborate with team members in real-time from any location.
Tips for ensuring compliance with updated forms
To ensure compliance with the updated medical necessity forms, healthcare providers should adopt best practices for completion. Common pitfalls include overlooking required documentation or misinterpreting guidelines, leading to claims denials. Therefore, it is crucial to follow a checklist of mandatory elements needed for submission.
Required documentation often includes clinical notes, treatment history, and other relevant evidence that supports the necessity of the requested services or equipment like DME. Additionally, teams should foster communication across departments — including billing, clinical staff, and administrative individuals — to streamline processes.
Tracking changes and staying informed about future updates will be key. Subscribe to newsletters from organizations like CMS to receive ongoing information about any new shifts in documentation requirements.
Tools and resources for managing medical necessity forms
Utilizing a robust set of tools can greatly ease the management of medical necessity forms. pdfFiller offers interactive tools designed to simplify the filing and updating processes of these essential documents. Features like eSignature integration streamline the signing process, while collaboration tools promote teamwork among healthcare staff, ensuring forms are completed accurately and in a timely manner.
Furthermore, cloud-based solutions provide accessibility from anywhere, making it easier for teams to review and edit documentation on the go. With pdfFiller, healthcare providers can cater to the evolving needs of their practices by leveraging these innovative capabilities for better efficiency and compliance.
Frequently asked questions (FAQs)
One of the most common reasons for claim denials related to medical necessity forms is failure to provide adequate documentation to substantiate the necessity of the requested services. Insufficient detail often raises questions during the review process, leading to rejections.
Providers can stay informed about ongoing changes in documentation requirements by subscribing to resources from organizations like CMS or healthcare associations. Regular training sessions and workshops can also keep teams updated. It's essential to review forms regularly to ensure they're aligned with current regulations and practices.
Keeping medical necessity forms updated is crucial for compliance and workflow efficiency. Outdated forms not only risk claims rejections due to incomplete information but can also hinder the overall patient care experience, potentially delaying access to necessary treatments.
Special considerations for different healthcare settings
Different healthcare settings, such as hospitals and private practices, require tailored approaches to medical necessity forms. Hospitals may have broader protocols due to their variety of departments and patient types. In contrast, private practices might focus on more specialized treatments, requiring distinct considerations in forms related to specific specialties, such as telemedicine or DME.
For example, telemedicine forms now typically include fields reflecting virtual assessments that necessitate distinct evaluations from in-person visits. This illustrates the need for ongoing adaptation to ensure the appropriate forms bring clarity and comply with updated regulations.
Best practices for training staff on new requirements
Training staff on the new requirements for medical necessity forms is essential to ensure compliance and accuracy. Healthcare organizations should utilize various training resources available through tools like pdfFiller to enhance their teams’ understanding of form requirements. Interactive training modules can engage staff effectively.
Creating a knowledge base for ongoing education allows staff to access information when needed, promoting a culture of learning and readiness. Additionally, facilitating team workshops and meetings helps reinforce best practices and encourages open dialogue regarding challenges faced during form completion.
Success stories: organizations that effectively adapted to changes
Several healthcare organizations have successfully implemented new medical necessity forms, yielding positive outcomes in their operations and patient satisfaction. For instance, a community hospital recently revamped its documentation process by utilizing pdfFiller to automate part of its paperwork, resulting in a decrease in claims denial rates by over 30%.
Key takeaways from innovating healthcare leaders include the importance of training staff on new protocols and using technology to streamline workflows. By harnessing modern solutions like pdfFiller for document management, organizations can improve overall efficiency and ensure compliance with updated regulations.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit changes to medical necessity in Chrome?
Can I edit changes to medical necessity on an iOS device?
How do I complete changes to medical necessity on an Android device?
What is changes to medical necessity?
Who is required to file changes to medical necessity?
How to fill out changes to medical necessity?
What is the purpose of changes to medical necessity?
What information must be reported on changes to medical necessity?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.















