Get the free Hmsacom - Prior Authorization Request
Get, Create, Make and Sign hmsacom - prior authorization
Editing hmsacom - prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out hmsacom - prior authorization
How to fill out hmsacom - prior authorization
Who needs hmsacom - prior authorization?
HMSAcom - Prior Authorization Form: A Comprehensive Guide
Understanding prior authorization
Prior authorization is a critical component in the healthcare system, acting as a cost-saving mechanism designed to ensure that specific medications, treatments, or procedures are medically necessary before patients receive them. This process can involve the healthcare provider, the patient, and the insurance company, effectively serving as a gatekeeper to control costs and ensure appropriateness of care.
The significance of prior authorization extends beyond mere cost management; it plays a vital role in safeguarding patients from unnecessary services or treatments. By requiring providers to demonstrate the necessity of a service, health plans aim to prevent abuse and ensure that patients receive care that aligns with recommended clinical guidelines.
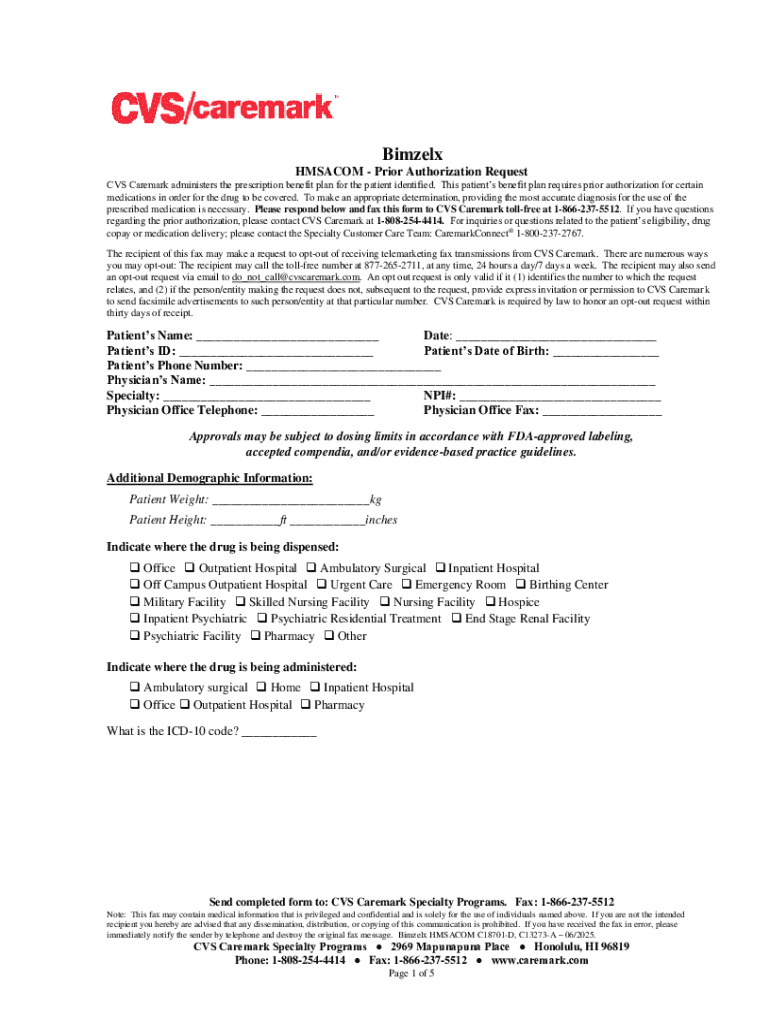
Overview of the HMSA prior authorization form
The HMSA (Hawaii Medical Service Association) prior authorization form is a standardized document that facilitates the request for coverage on specific medical services or treatment plans. This form is not only a requirement but also serves a critical function in communicating necessary details between healthcare providers and the insurance company.
The primary purpose of this form is to gain approval from HMSA before treatment begins, ensuring that both the provider and the insurer are aligned on the medical necessity of the requested service. Without this approval, providers may risk providing services that are not reimbursed by the health plan, thereby creating financial burdens on patients.
Preparing to fill out the HMSA prior authorization form
Before filling out the HMSA prior authorization form, it’s crucial to gather all necessary documentation. This preparation not only streamlines the process but also enhances the chances of a successful approval. Relevant materials can include detailed medical records, a comprehensive treatment plan, and any previous authorization letters that may aid the current request.
Understanding the specific requirements outlined by HMSA is essential. Each insurance provider may have unique documentation needs, information format, and submission guidelines. Being familiar with these can significantly expedite the authorization process and mitigate the risk of administrative errors.
Step-by-step instructions for completing the HMSA form
Filling out the HMSA prior authorization form requires attention to detail to ensure that all information provided is accurate and complete. Here’s a step-by-step guide to help navigate the sections of the form efficiently.
Section 1: Patient information
In this section, you’ll need to provide comprehensive details about the patient, including their full name, date of birth, and insurance identification number. Ensure that all formatting aligns with HMSA's guidelines; for example, using the correct initial capitalization in names and proper date formats.
Section 2: Provider information
Accurate provider details are crucial as this section identifies who is requesting the prior authorization. Include the provider’s name, NPI (National Provider Identifier) number, and contact information. Errors in this section can lead to frustrating communication delays.
Section 3: Insurance information
In the insurance information section, ensure to double-check that the patient’s policy number and group information are entered correctly. Common mistakes include typos in policy numbers or failing to update information if the patient’s coverage has changed.
Section 4: Medical necessity justification
This is a critical section where you must convincingly justify the medical necessity of the requested service. Use clinical evidence, treatment guidelines, and previous patient history to craft a compelling argument. Pay attention to the phrasing as HMSA’s reviewers need to quickly understand the rationale behind the request.
Section 5: Additional comments
The additional comments section allows for any further context or justification for the request that hasn’t been covered in previous sections. This is particularly useful when the patient has unique circumstances that warrant special consideration.
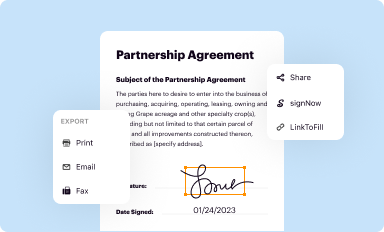
Editing, signing, and submitting the form
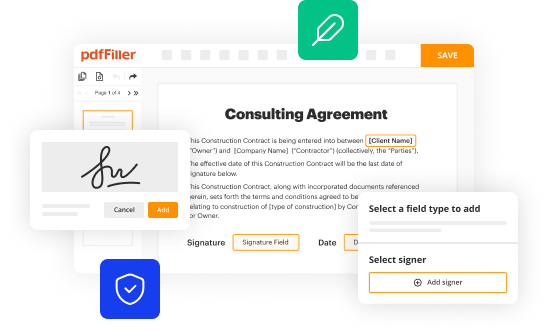
Once the HMSA prior authorization form is completed, it’s important to review it thoroughly. Harness pdfFiller’s tools for editing to ensure all entries are clear and accurate. Pay particular attention to sensitive information; ensuring no confidential details are omitted or erroneous.
When it comes to signing the form, electronic signatures are a convenient option offered by pdfFiller. Follow the straightforward steps to add your signature electronically to ensure that you comply with all necessary legal requirements.
After signing, always save your work. Using pdfFiller's cloud-based system, you can easily manage your documents. When ready to submit, you often have the option to submit the form either through HMSA’s online portal or via linked third-party platforms that are compatible.
Common challenges with the HMSA prior authorization form
Navigating the HMSA prior authorization form can present challenges. Common issues arise from incomplete information or misunderstandings regarding HMSA's requirements. A frequent point of confusion involves the medical necessity justification; many providers find it daunting to assert the appropriate rationale convincingly.
Additionally, difficulties with administrative follow-up can make the process cumbersome. Patients and providers alike often express frustration in the time it takes to receive a response regarding their request. Clear communication with the insurance representatives can significantly ease this process.
Following up after submission
After submitting the HMSA prior authorization form, it’s beneficial to proactively check the status of your request. Most insurers provide a tracking option within their online portals. Understanding typical timeframes for authorization decisions can help manage patient expectations.
In the unfortunate event that a request is denied, it's essential to be prepared to take action. This might involve reviewing the denial letter for specifics, gathering additional documentation that supports the medical necessity, and outlining a clear plan for appeal.
Additional resources for users of the HMSA prior authorization form
For further assistance with the HMSA prior authorization form and process, various resources are available. Contacting HMSA support directly can provide personalized assistance tailored to your needs. Additionally, exploring informative blogs and articles can offer insights into best practices for successfully navigating authorization requests.
Community forums present another avenue where individuals can share experiences, exchange tips, and gain perspective from others who have also navigated similar paths. Engaging with these platforms can help demystify the process and provide a support network.
Interactive tool: Track your prior authorization request
Using pdfFiller's tracking features can significantly enhance the management of your prior authorization requests. The platform allows users to monitor the status of submissions and receive alerts for any changes. Setting up notifications ensures that no important updates are missed, equipping users with the necessary information to act promptly when needed.
Alternatives to the HMSA prior authorization process
While the HMSA prior authorization process follows a specific format, other insurance providers have their own unique requirements and procedures. Understanding these differences is crucial for healthcare providers and patients to facilitate proper planning and avoid surprises during the authorization process.
Best practices across various health plans often include utilizing streamlined forms that simplify the communication process, ensuring essential details are always highlighted, and providing supportive documentation. Awareness of these practices can offer insights into improving your approach and ensuring more efficient submissions.
Personal stories: How prior authorization affects patients
Hearing from individuals who have navigated the HMSA prior authorization process can provide valuable insight into its real-life implications. Personal stories shed light on the emotional and physical strains that can accompany the wait for authorization, illustrating why thorough preparation and knowledge are essential.
Testimonials from patients who have successfully navigated the process often highlight the importance of clear communication with healthcare providers, timely follow-ups, and the impact of ongoing support from family and community. Sharing these narratives exemplifies the human side of healthcare bureaucracy and emphasizes the need for efficient processes.
User insights and feedback
Evaluating user experiences with the HMSA prior authorization form can guide future enhancements. Through feedback, organizations can identify pain points that need to be addressed, making the process smoother and more user-friendly for providers and patients alike.
Encouraging feedback loops—including surveys, forums, and direct outreach—can facilitate productive discussions about how the form and submission process can adapt to better meet users' needs. Each piece of feedback represents an opportunity for continuous improvement.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find hmsacom - prior authorization?
How do I edit hmsacom - prior authorization online?
How do I edit hmsacom - prior authorization straight from my smartphone?
What is hmsacom - prior authorization?
Who is required to file hmsacom - prior authorization?
How to fill out hmsacom - prior authorization?
What is the purpose of hmsacom - prior authorization?
What information must be reported on hmsacom - prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.