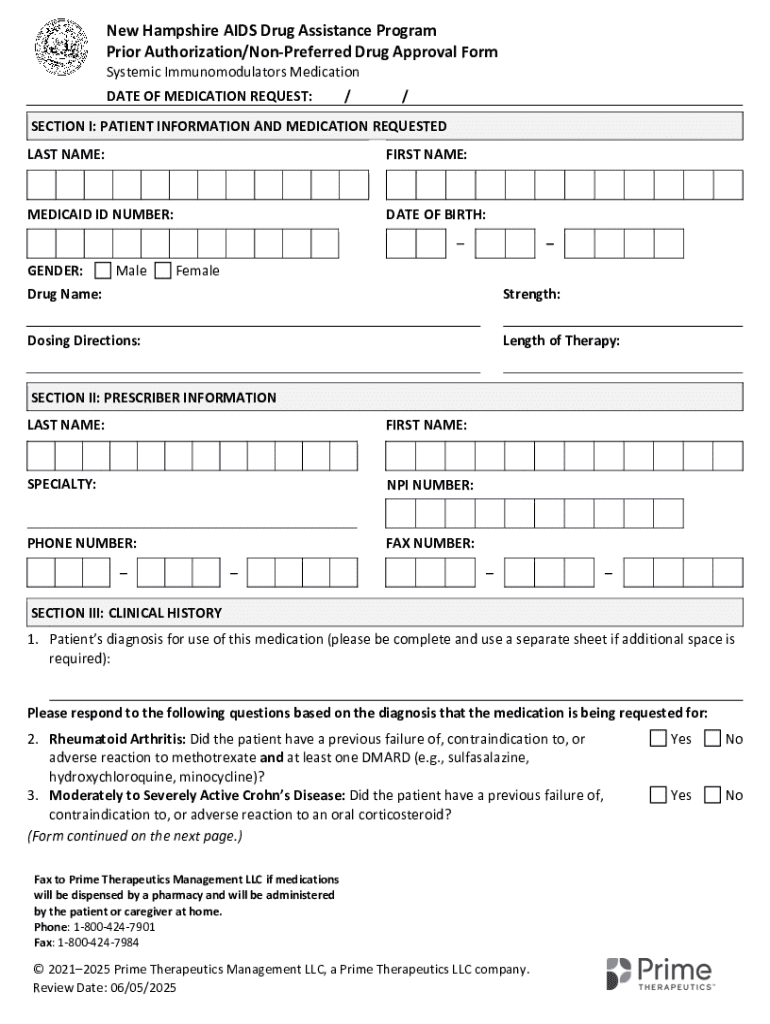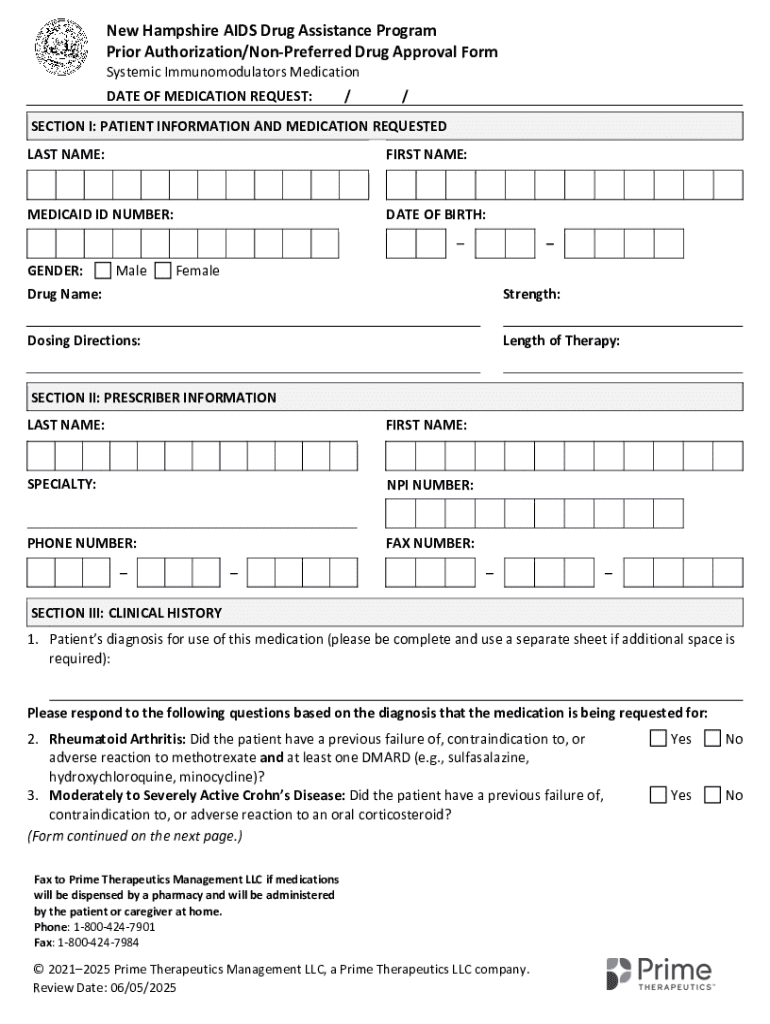
Get the free Prior Authorization/non-preferred Drug Approval Form
Get, Create, Make and Sign prior authorizationnon-preferred drug approval
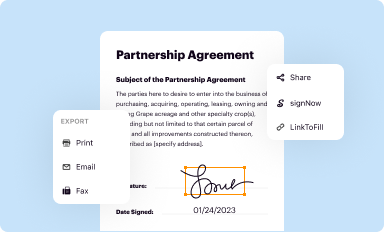
Editing prior authorizationnon-preferred drug approval online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorizationnon-preferred drug approval
How to fill out prior authorizationnon-preferred drug approval
Who needs prior authorizationnon-preferred drug approval?
Understanding the Prior Authorization Non-Preferred Drug Approval Form
Understanding prior authorization: Key concepts
Prior Authorization (PA) is a process used by health insurers to determine whether a specific treatment, service, or medication is medically necessary before it is provided to the patient. This mechanism is especially vital when it comes to approving certain medications that may not be on the insurer’s preferred list. PA plays a significant role in healthcare as it helps control costs and ensure that patients receive appropriate care. In this landscape, it is crucial to differentiate between preferred and non-preferred drugs. Preferred drugs are typically those the insurance plan encourages due to cost-effectiveness, while non-preferred drugs may require additional steps for approval due to higher costs.
The Non-Preferred Drug Approval Process generally involves submitting a specific form that outlines the need for a drug that is not on the insurer’s preferred list. Patients and providers alike need clarity on this process, as it can greatly impact treatment timelines and patient health outcomes.
The role of non-preferred drug approval forms
The Non-Preferred Drug Approval Form serves several essential purposes. Its primary function is to provide insurers with necessary details about the patient’s health condition and the rationale for prescribing a non-preferred medication. This ensures that insurers have the information required to determine the medical necessity of the drug and support the approval process.
A Non-Preferred Drug Approval Form is typically required in scenarios where a prescribed medication is not on the patient's insurance formulary. Such situations might include changing therapies due to inadequate responses to preferred drugs or specific patient allergies that contraindicate the use of standard alternatives. Without this form, patients may face delays in access to critical medications, impacting their health outcomes.
Step-by-step guide to completing the non-preferred drug approval form
Completing a Non-Preferred Drug Approval Form can be a straightforward process if you approach it methodically. Below is a step-by-step guide that can help streamline your submissions.
Important considerations and criteria for approval
Insurers typically evaluate requests for non-preferred drugs based on established medical guidelines and criteria. Common factors include the patient’s medical history, previous medication trials, and the rationale provided for the necessary use of the non-preferred drug over preferred alternatives.
Typical reasons for approval can involve documented failures with preferred therapies or specific medical conditions that strictly require the non-preferred option. Conversely, requests may be denied for lack of adequate supporting documentation or if the insurer deems the prescribed medication unnecessary. Being prepared can aid in this process; extra documentation might be required for certain cases.
In cases of denial, understanding the appeal processes is critical. Submitting additional evidence or clarifying points can often turn a denial into an approval when navigating through the complexities of insurer responses.
Tracking and managing your submission
Once the Non-Preferred Drug Approval Form is submitted, tracking the status of your application becomes vital. Many insurance companies offer online portals to check the status of submissions, which can help you stay informed on a turnaround time.
Budgets and treatment necessities can fluctuate, so timeliness is crucial. If you experience delays, consider proactive communication with the insurer to clarify and expedite the approval. Documenting all correspondence can provide useful references if issues arise later.
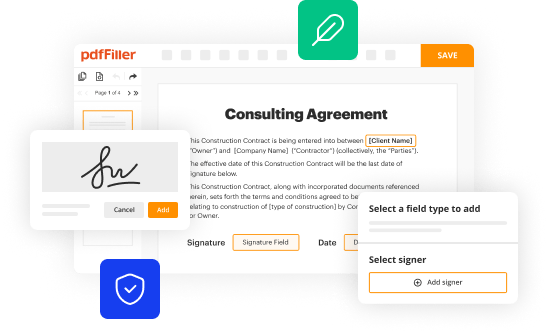
Utilizing pdfFiller for form management
pdfFiller brings an efficient solution to managing your Non-Preferred Drug Approval Form. The platform allows users to access the form online easily and utilize interactive tools to enhance the filling process. This means you can create, edit, and modify your form quickly, ensuring all information is up-to-date.
FAQs related to non-preferred drug approval
When navigating the landscape of Non-Preferred Drug Approval, various questions frequently arise. Common inquiries might focus on the timeline for approvals, coverage specifics, and nuances in terminology surrounding the process.
Patients and providers should seek clarity on all aspects of the form submission process. Reliable resources are available through insurance providers or healthcare forums, which can shed light on the common hurdles faced when dealing with non-preferred drug approvals.
Best practices for expediting approvals
To avoid delays in the Non-Preferred Drug Approval process, consider implementing several best practices. Clear communication with insurers is crucial; provide them with all requested information upfront to minimize back-and-forth correspondence.
Additionally, leveraging technology—like pdfFiller—can streamline your workflow for form submission, ensuring quick corrections and updates can be made as needed. Health professionals often emphasize documenting interactions with insurance companies, which can be beneficial if issues arise later on.
Case studies: Successful non-preferred drug approvals
Real-life examples provide invaluable insights into the Non-Preferred Drug Approval process. One case study may involve a patient needing a specific medication after experiencing adverse effects from several preferred options.
In another instance, the complexity of an approval may stem from a patient's unique medical history, demonstrating the necessity for thorough documentation and clear justification on the part of the prescriber. These case studies underline the importance of careful planning and understanding health plan policies, which can lead to successful outcomes in complex scenarios.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I sign the prior authorizationnon-preferred drug approval electronically in Chrome?
How can I edit prior authorizationnon-preferred drug approval on a smartphone?
How do I edit prior authorizationnon-preferred drug approval on an Android device?
What is prior authorization non-preferred drug approval?
Who is required to file prior authorization non-preferred drug approval?
How to fill out prior authorization non-preferred drug approval?
What is the purpose of prior authorization non-preferred drug approval?
What information must be reported on prior authorization non-preferred drug approval?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.