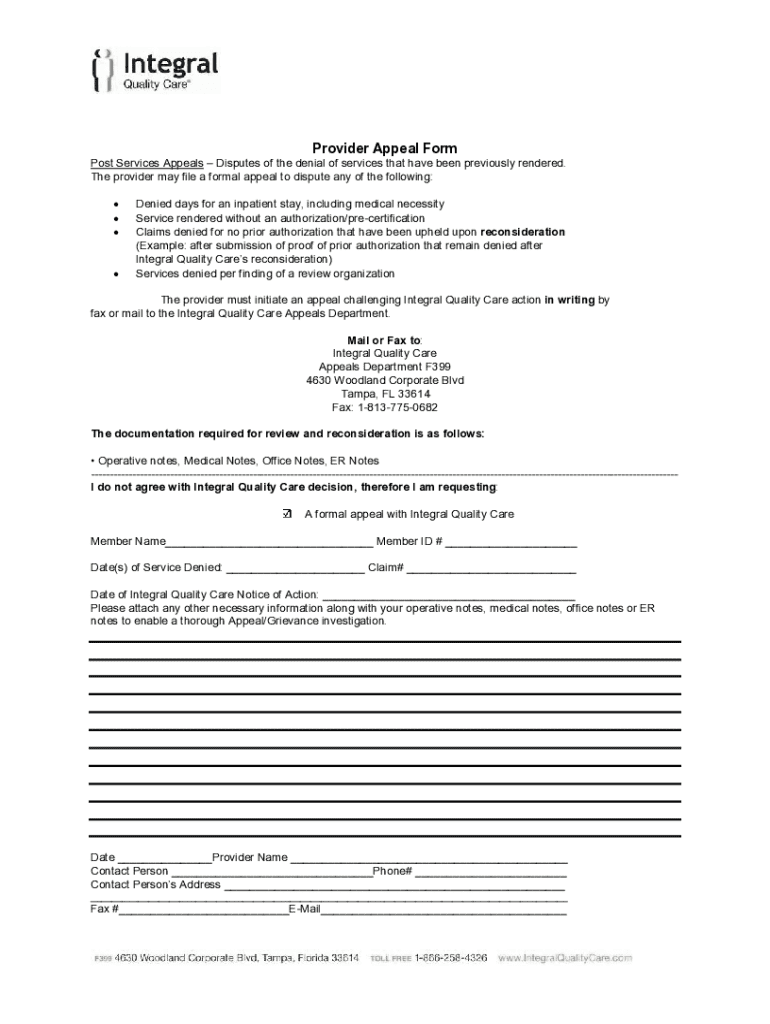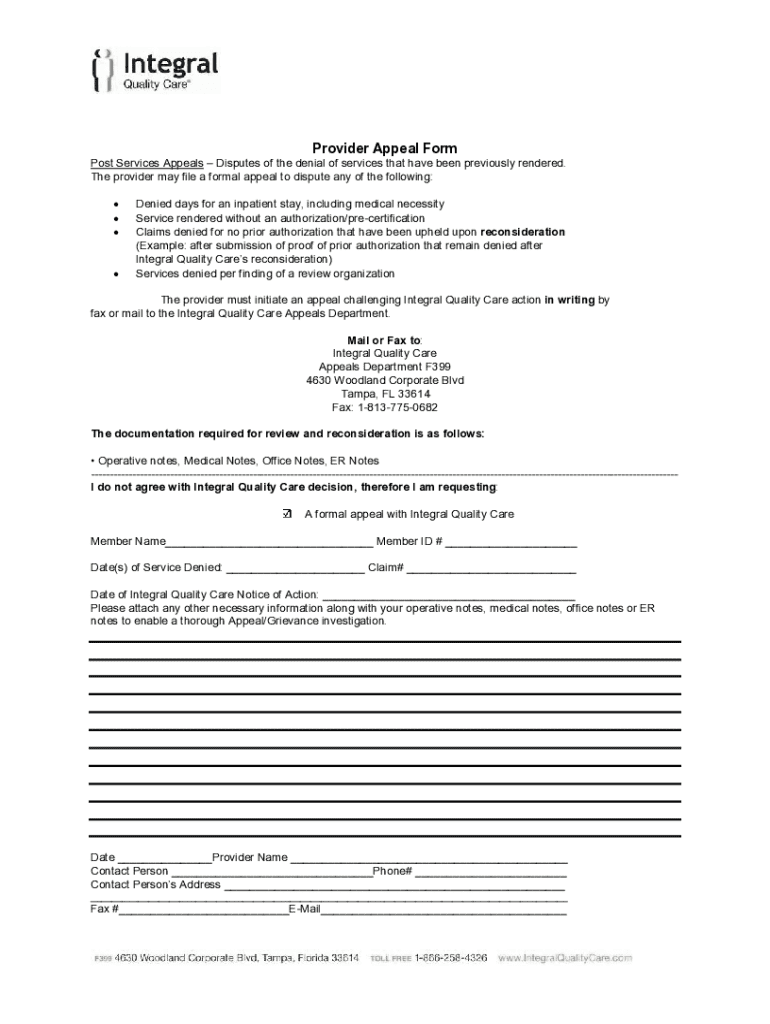
Get the free Provider Appeal Form
Get, Create, Make and Sign provider appeal form
How to edit provider appeal form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out provider appeal form
How to fill out provider appeal form
Who needs provider appeal form?
A Comprehensive Guide to the Provider Appeal Form
Understanding the provider appeal form
A provider appeal form is a formal document submitted by healthcare providers when they disagree with a decision made by an insurance company or healthcare plan. This form initiates the appeal process, allowing providers to contest denials of claims or other administrative decisions that affect patient care. In many scenarios, this form is a critical step for ensuring that healthcare providers are properly reimbursed and that patients receive the necessary coverage.
The importance of the provider appeal form cannot be understated. It serves as a mechanism through which providers can exercise their appeal rights, ensuring they have a voice in the reimbursement process. In many cases, the appeal may resolve disputes over coverage denials or underpayments, which can significantly affect both the provider's revenue and patient care. Understanding this form is crucial for healthcare providers who want to navigate the complex world of healthcare billing effectively.
Preparing to fill out the provider appeal form
Before diving into the process of completing a provider appeal form, it’s essential to gather the necessary information. This involves collating details such as the patient's name, insurance information, and details regarding the initial claim that was denied. This step is crucial as it streamlines the appeal process and ensures that all required information is at hand when filling out the form.
In addition to patient details, providers must include their own information, such as provider identification numbers and contact details. It's also essential to provide specifics of the appeal itself, including relevant dates, coding used in the original submission, and any references to policies that support the appeal. Understanding eligibility for filing an appeal is another critical component. Not every denial qualifies for an appeal; being familiar with the criteria will help providers efficiently determine whether they should proceed.
Step-by-step instructions for completing the provider appeal form
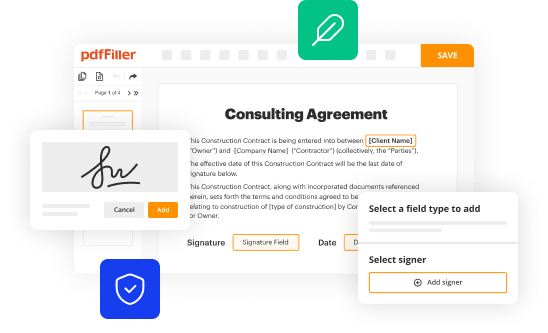
The first step in completing the provider appeal form is accessing the document. This can typically be done by downloading the form from pdfFiller or through your healthcare provider's portal. pdfFiller offers multiple options for accessing this form, including online access, which allows for easy completion from any device.
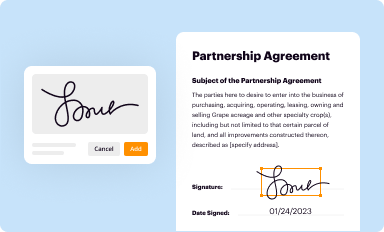
When filling out the provider appeal form, begin with the personal and provider information section. Here, accuracy is vital. Next, provide a clear and concise appeal description, outlining the reason for the appeal. Be sure to attach any supporting documentation that may bolster your case. Typically, this could include previous correspondence, medical records, or treatment plans that may justify the appeal. Finally, remember to sign and date the form before submission.
Utilizing interactive tools within pdfFiller can also greatly enhance the appeal process. Real-time editing features allow for corrections on the fly, and using eSignature integration means it's easier than ever to complete and send off your appeal in a timely manner.
Common mistakes to avoid while filling out the form
Filling out a provider appeal form can be straightforward, but there are common pitfalls that can lead to the form being rejected or delayed. One of the most frequent mistakes is providing incomplete information; every field must be filled accurately to ensure the appeal is processed. Be vigilant about double-checking whether all required details are included.
Another common mistake is the submission of incorrect documentation. It's critical to include the right supporting documents that correspond with the details provided in your appeal description. Additionally, misunderstandings surrounding appeal procedures can lead to incorrect form filings. Always stay updated on the specific process and requirements outlined by the insurance provider.
Editing and finalizing your provider appeal form
Once you have filled out the provider appeal form, it’s time to review and double-check your information meticulously. Incorrect details can lead to delays or rejections of your appeal, so this is a crucial step in the process. pdfFiller offers a suite of editing tools that make this task easier. You can add comments, make necessary adjustments, or highlight sections to ensure everything is accurate and clearly presented.
If needed, you can utilize pdfFiller’s features to merge documents, which can be particularly useful if you are consolidating multiple pieces of supporting evidence. When everything is in order, save your completed form effectively, using appropriate file naming conventions for easy retrieval later on.
Submitting your provider appeal form
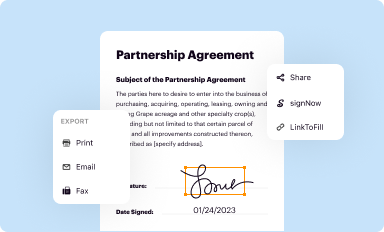
Submitting the provider appeal form can be done through several methods, depending on the requirements set by your insurance provider. Many providers now accept online submissions, which can expedite the process and provide a digital trail for your records. However, if online submission isn’t an option, mailing the appeal form is still a viable method.
After submission, tracking your appeal status is crucial. Many insurance companies provide an online portal where you can check the status of your appeal. This transparency can provide peace of mind and help you anticipate responses and timelines. Typically, after submitting your appeal, expect a response from the provider within a defined period, as specified in their policies.
Collaborating on appeals within teams
Collaboration can be fundamental in managing appeals effectively, especially within larger healthcare teams. pdfFiller facilitates this process with its collaborative features. By sharing the provider appeal form with colleagues, team members can provide feedback, make necessary adjustments, and ensure that the appeal is robust before submission.
Best practices for document management also play a critical role here. Organizing appeal documents by categorizing them based on patient names or case types can ease the retrieval process later on. Additionally, setting up alerts to notify team members of status updates on submitted appeals can keep everyone informed and engaged in the workflow.
Helpful resources for providers
For healthcare providers navigating the complexities of filing appeals, several resources can prove invaluable. Frequently asked questions (FAQs) about the provider appeal form can assist in addressing common queries. Additionally, links to relevant regulatory bodies and guidelines can offer deeper insights into best practices and expectations in the appeal process.
Furthermore, maintaining contact with support representatives from the insurance company can clarify any uncertainties regarding appeals. Having access to direct lines of communication can help resolve issues quickly and ensure that appeals are filed correctly.
Sign up for updates on managing provider appeals
Staying informed about changes in the appeal process, new regulations, and best practices can significantly enhance your ability to manage provider appeals effectively. Sign up for email updates via pdfFiller can ensure you receive timely information directly related to your work, keeping you ahead in an ever-evolving field.
By taking proactive measures to stay informed, you can better support your patients and navigate the complexities of the healthcare landscape. Engaging with these updates can help providers advocate for themselves and their patients more effectively, ensuring that necessary care is accessible and fairly reimbursed.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my provider appeal form in Gmail?
Where do I find provider appeal form?
How do I edit provider appeal form online?
What is provider appeal form?
Who is required to file provider appeal form?
How to fill out provider appeal form?
What is the purpose of provider appeal form?
What information must be reported on provider appeal form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.