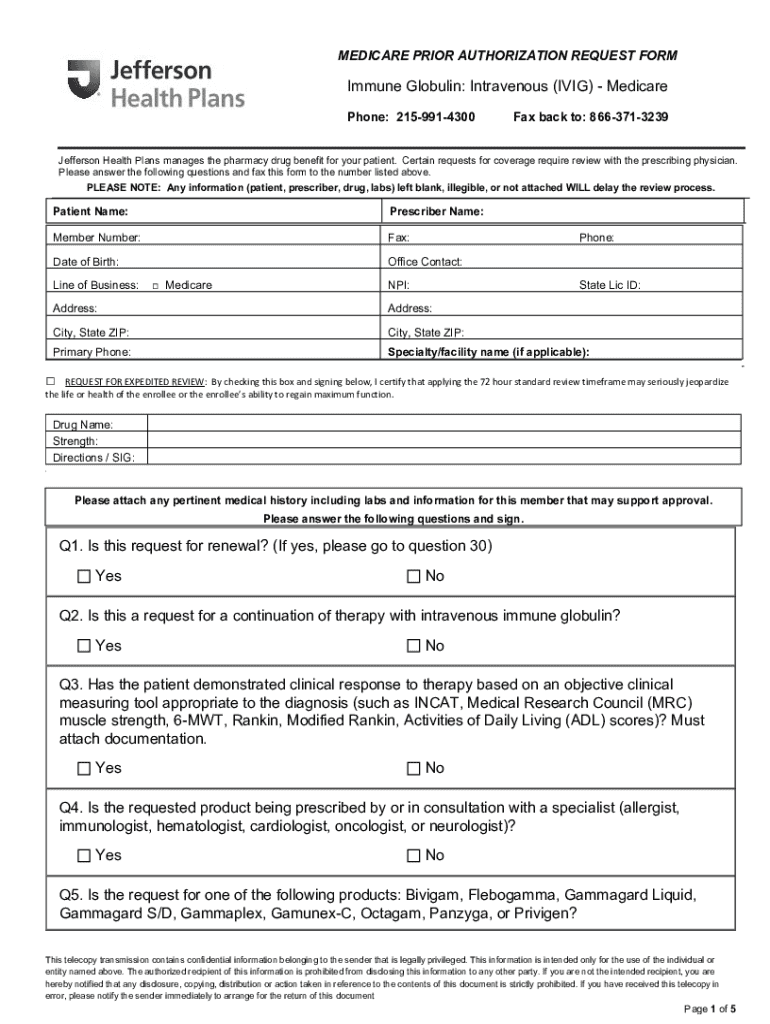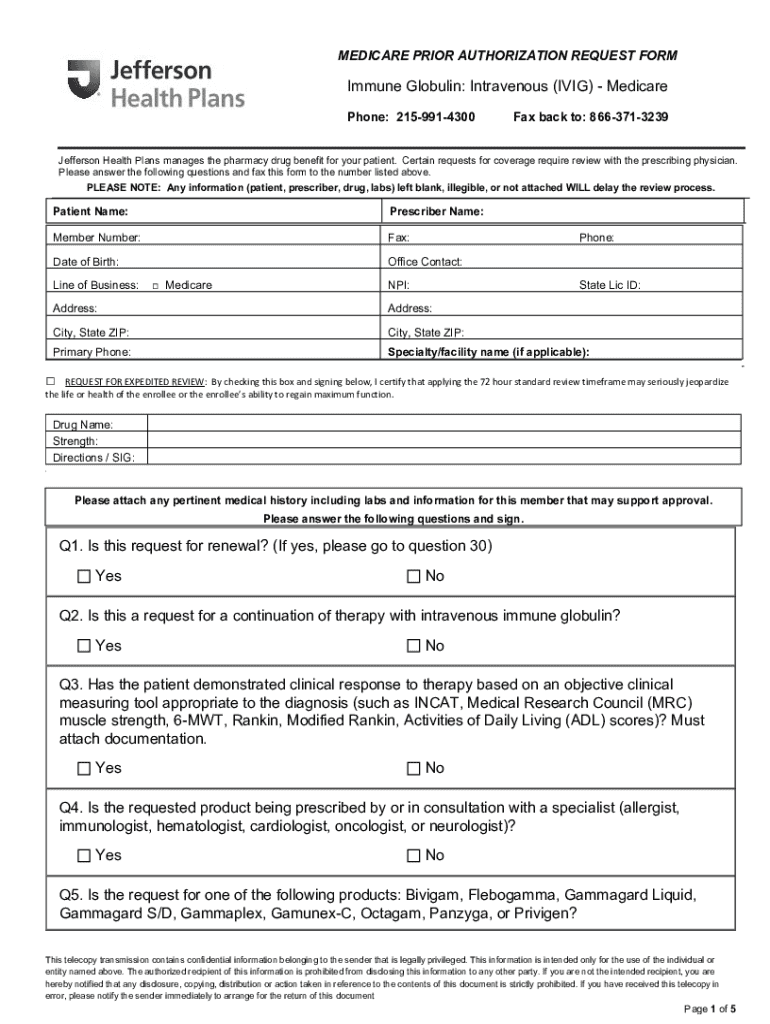
Get the free Medicare Prior Authorization Request Form
Get, Create, Make and Sign medicare prior authorization request
Editing medicare prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medicare prior authorization request
How to fill out medicare prior authorization request
Who needs medicare prior authorization request?
Medicare Prior Authorization Request Form: A Comprehensive Guide
Understanding Medicare prior authorization
Medicare prior authorization is a crucial process intended to ensure that patients receive medically necessary services and treatments covered by Medicare. It serves as a safeguard against inappropriate or unnecessary healthcare, ultimately enhancing patient safety and care quality.
Prior authorization acts as a checkpoint where healthcare providers must obtain approval from Medicare before delivering specific services or procedures. This approval helps to confirm that the proposed services align with Medicare's coverage guidelines and are deemed necessary for the patient's diagnosed condition.
Types of services requiring prior authorization
Medicare requires prior authorization for a variety of services, ensuring that they are medically necessary and appropriate. Some common types include:
Overview of the Medicare prior authorization request form
The Medicare prior authorization request form is a structured document designed to collect essential information about the patient, the provider, and the requested services. Completing this form accurately is vital to ensure seamless processing of the authorization request.
Step-by-step guide: completing the Medicare prior authorization request form
Completing the Medicare prior authorization request form can be simplified by following these structured steps. Ensuring accuracy is key in avoiding delays or denials.
Step 1: Gather Necessary Information. To complete the request form effectively, collect all necessary documentation, including:
Step 2: Fill Out the Form Accurately. Ensure that every section of the form is filled out correctly, paying special attention to common mistakes, such as misspelling names or incorrect insurance numbers.
Step 3: Review Your Submission. Before submission, double-check all information provided to ensure its accuracy. Key areas to review include patient and provider information.
Step 4: Submit the Request Form. Depending on your preference, submit your form online, by mail, or via fax. Once submitted, track your submission status for any updates.
Interacting with Medicare: after submission
After submission of your Medicare prior authorization request form, understanding the approval process is essential. Typically, you can expect a notification from Medicare regarding the approval or denial of your request within a specific timeframe.
Should there be delays or denials, first identify the reasons for denial, which might include insufficient documentation or failure to meet medical necessity criteria. In cases of denial, you can file an appeal, which requires gathering further justification for the requested services.
Tools and resources available
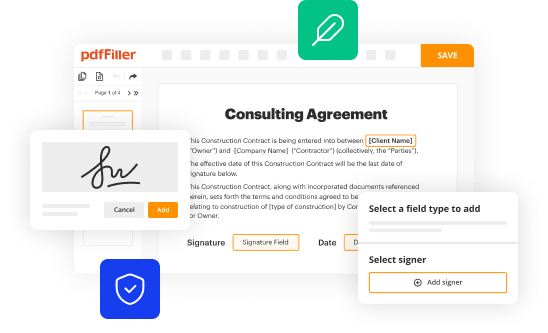
Utilizing effective tools can significantly streamline the process of managing the Medicare prior authorization request form. For instance, pdfFiller offers a comprehensive suite of document management features that enhance productivity.
Best practices for using the Medicare prior authorization request form
To maximize the efficiency of the Medicare prior authorization request process, consider implementing best practices that focus on organization and communication.
FAQs on Medicare prior authorization request form
Many individuals and teams may have questions regarding the Medicare prior authorization request form, especially if they are first-time users. Understanding common inquiries can enhance confidence in navigating the process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete medicare prior authorization request online?
How do I edit medicare prior authorization request online?
Can I sign the medicare prior authorization request electronically in Chrome?
What is medicare prior authorization request?
Who is required to file medicare prior authorization request?
How to fill out medicare prior authorization request?
What is the purpose of medicare prior authorization request?
What information must be reported on medicare prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.