A Comprehensive Guide to the MaineCare Prior Authorization Request Form
Understanding MaineCare and prior authorization
MaineCare is Maine's Medicaid program, designed to provide healthcare coverage for low-income residents, including families, the elderly, and individuals with disabilities. It plays a critical role in ensuring access to necessary medical services and supports the overall health of the community. Prior authorization is an essential part of this process, allowing healthcare providers to request approval for specific services or treatments before they are administered.
The importance of prior authorization cannot be overstated, as it helps control healthcare costs while ensuring that patients receive the appropriate care. Without prior authorization, services may not be covered under MaineCare, leading to unexpected expenses for patients and providers. Understanding eligibility requirements is crucial as well; not everyone qualifies for MaineCare, and not all services require prior authorization.
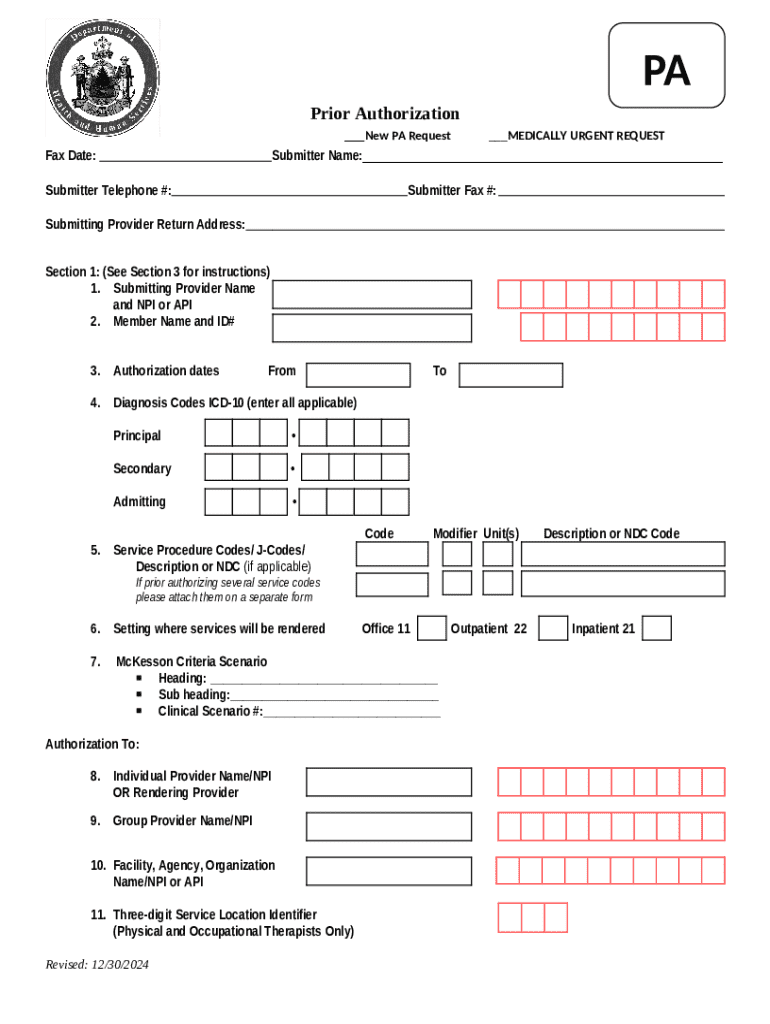
Introduction to the MaineCare prior authorization request form
The MaineCare Prior Authorization Request Form serves as a formal request for healthcare providers to gain approval for specific medical services, procedures, or medications covered under MaineCare. This form is essential as it establishes the medical necessity of the requested services and helps streamline the approval process.
Typically, the form is required when a provider believes that a service, such as an MRI or specialist consultation, is necessary for the patient's treatment plan. Before starting to fill out the form, healthcare providers should gather essential information, including patient demographics, provider details, and specifics about the services being requested.
Accessing the MaineCare prior authorization request form
Locating the MaineCare Prior Authorization Request Form is straightforward. The form is available on the Maine Department of Health and Human Services website, where it can be accessed by navigating to the MaineCare section and selecting the appropriate link for prior authorization requests.
It's crucial to use the most recent version of the form to avoid delays or issues with your submission. Older forms may not comply with current guidelines and could lead to rejections.
Detailed walkthrough of the form sections
Section 1: Patient information
This section requires detailed personal information about the patient, including full name, date of birth, and MaineCare ID number. Providing accurate information is vital, as any discrepancies can lead to complications during the authorization process.
Section 2: Provider information
In this section, healthcare providers must include their name, contact details, and MaineCare provider number. Verifying provider credentials is essential to ensure the legitimacy of the request and to streamline the authorization process.
Section 3: Service information
This part of the form specifies the services being requested, which can include various medical procedures such as diagnostic imaging, surgical interventions, or specialist referrals. It's critical to adhere to guidelines regarding which services require prior authorization.
Section 4: Medical justifications
Medical justifications are a cornerstone of the prior authorization process. This section should include clinical documentation that supports the need for the requested services, along with specific examples that reflect accepted justifications for treatment.
Section 5: Signatures and dates
This final section mandates signatures from both the provider and the patient (if applicable), along with the date of submission. Timeliness is key; delays in signing and submitting the form can result in slower processing times and can delay necessary care.
How to edit and customize your MaineCare prior authorization form
Editing the MaineCare Prior Authorization Request Form can be streamlined using pdfFiller’s powerful editing tools. With this platform, users can easily make necessary adjustments to the form without needing printouts or manual changes.
Open the form in pdfFiller's editor.
Utilize annotation tools to highlight or add comments.
Collaborate with team members in real-time to ensure all information is accurate and comprehensive.
This flexibility not only saves time but also enhances the accuracy of the submitted request, as changes can be made quickly and efficiently, reducing the chances of errors.
Submitting the MaineCare prior authorization request form
Submitting the completed MaineCare Prior Authorization Request Form can be done in several ways, primarily online or via traditional mail. Online submissions often expedite the processing time, while mail submissions average longer waiting periods for approval.
Submit through the MaineCare portal for faster processing.
Send the completed form to the designated authority address for processing.
Understanding the timelines for approval is crucial. Typically, providers can expect a response within a few days to a week; however, complex cases may take longer. You can track your submission status through the MaineCare provider portal.
Common mistakes to avoid
Filling out the MaineCare Prior Authorization Request Form can be daunting, and there are several common pitfalls that can lead to delays or denials. Ensuring accurate and complete information is vital. Common mistakes include incorrect patient identifiers, missing supporting documentation, and failing to obtain necessary signatures.
Double-check personal details for accuracy.
Confirm all required documentation is included.
Ensure signatures and dates are properly filled out before submission.
Taking the time to double-check your application before submitting can prevent these common errors and facilitate a smoother authorization process.
FAQs about the MaineCare prior authorization process
After submitting the MaineCare Prior Authorization Request Form, you may wonder what happens next. Typically, you will receive a notification regarding the approval or denial status.
Providers will receive a confirmation of receipt and a decision based on submitted information.
Providers can submit an appeal by gathering additional documentation and resubmitting the request.
Contact the MaineCare customer service for help with process-related inquiries.
Being aware of these options can help manage expectations and guide providers through the often complex MaineCare authorization landscape.
Leveraging pdfFiller for document management
Using pdfFiller offers significant advantages in managing healthcare forms like the MaineCare Prior Authorization Request Form. As a cloud-based document solution, pdfFiller allows users to access their forms from anywhere and on any device, ensuring flexibility and convenience.
Securely sign documents online, eliminating the need for physical signatures.
Work on forms in real-time with team members, enhancing accuracy and teamwork.
Store all healthcare forms in one place, making it easier to retrieve and manage documents as needed.
Overall, pdfFiller empowers users to optimize their document management processes, ensuring that essential forms like the MaineCare Prior Authorization Request Form are handled efficiently.
Final tips for a successful prior authorization experience
Effective communication between healthcare providers and patients is crucial for a successful prior authorization experience. Keeping patients informed about the necessity of their treatment, facilitating the gathering of required documentation, and ensuring forms are submitted promptly are all critical components.
Maintain a dialogue with patients about authorization and treatment plans.
Aim to submit requests as soon as possible to avoid last-minute issues.
Familiarize yourself with MaineCare's specific authorization guidelines to enhance success.
By following these best practices, healthcare providers can significantly improve their chances of obtaining timely authorization, ultimately leading to better patient care and satisfaction.