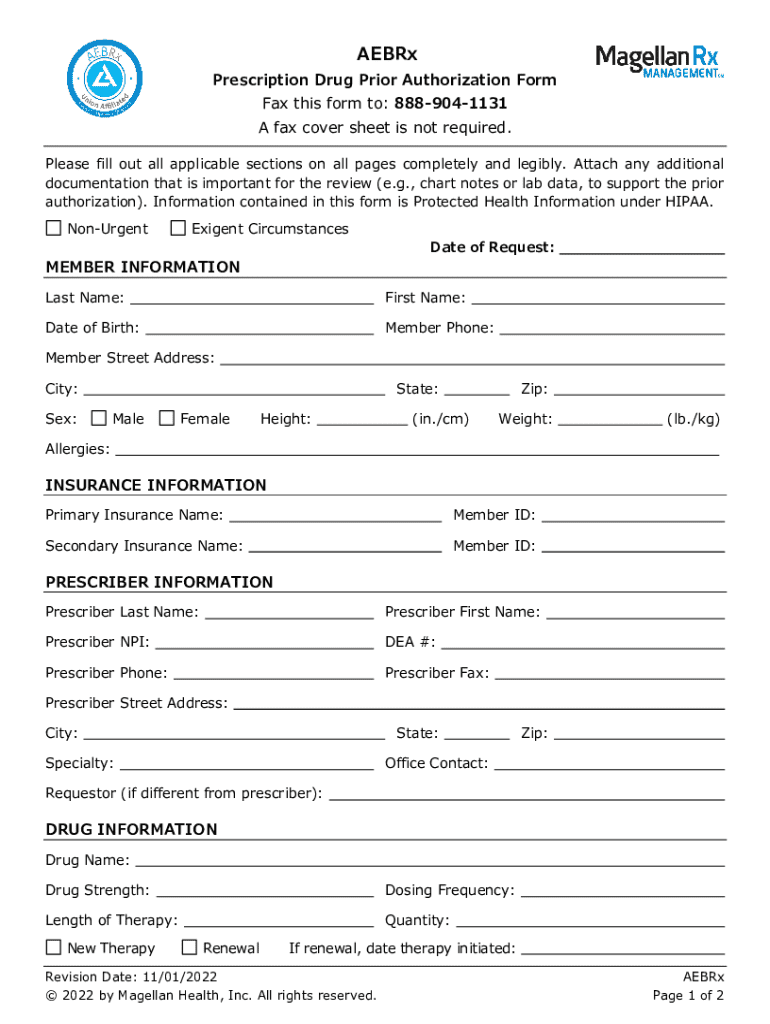
Get the free Aebrx Prescription Drug Prior Authorization Form
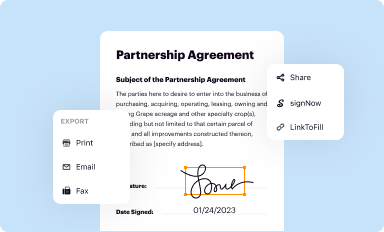
Get, Create, Make and Sign aebrx prescription drug prior
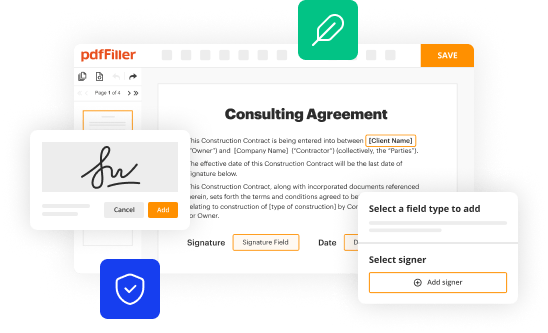
How to edit aebrx prescription drug prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out aebrx prescription drug prior
How to fill out aebrx prescription drug prior
Who needs aebrx prescription drug prior?
Aebrx prescription drug prior form: A comprehensive guide
Understanding the AEBRX prescription drug prior form
The AEBRX prescription drug prior form is a crucial document in the healthcare landscape. Designed for healthcare providers and patients, it serves as a request for prior authorization from insurance companies for specific medications. This process ensures that the drugs prescribed align with the insurer's guidelines, optimizing patient care while controlling costs.
The importance of the prior authorization process cannot be overstated. It acts as a safeguard in healthcare distribution, ensuring that prescribed medications are medically necessary and effective. For patients, this often means the difference between receiving timely treatment and encountering delays that could exacerbate health issues.
When is the AEBRX prescription drug prior form required?
Certain medications typically require this form due to their cost and the need for careful monitoring of their use. Drugs used for complex conditions, such as rheumatoid arthritis or specialty drugs for cancer treatments, often necessitate a prior authorization.
Physicians may need to submit the AEBRX form when prescribing these high-cost medications or those that pose significant health risks if misused. Additionally, specific insurance providers have unique criteria determining when prior authorization is mandatory, leading to variability in how and when this form is used across healthcare systems.
Step-by-step guide to completing the AEBRX prescription drug prior form
Completing the AEBRX prescription drug prior form requires careful attention to detail. Here is a breakdown of the essential steps:
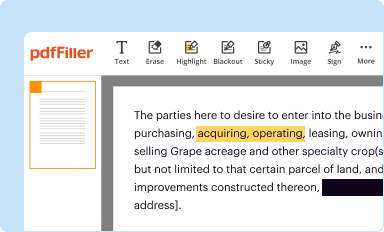
Using pdfFiller for managing the AEBRX form
pdfFiller stands out as a valuable resource for managing the AEBRX prescription drug prior form. This platform provides seamless editing and filling capabilities for PDF forms, giving users an accessible way to manage all their documentation needs in one place.
One of the standout features of pdfFiller is its collaboration tools, which allow multiple users within a healthcare team to work on forms concurrently. This facilitates better management of patient care and documentation requirements, offering a streamlined process that keeps everyone informed. Features like secure sharing, document signing solutions, and easy form access enhance the overall efficiency.
Common pitfalls and how to avoid them
Completing the AEBRX form efficiently requires diligence to avoid frequent mistakes that can lead to submission delays. Common issues include missing information, incorrect medication details, or indications not clearly stated. Ensuring that the form is completed thoroughly is essential to prevent setbacks.
To sidestep these pitfalls, providers should double-check each section of the form for completeness. It's wise to cross-verify medication names, dosages, and patient data before finalizing. Remember, legibility is crucial—if the insurer cannot read the response, it can lead to further complications.
FAQs about the AEBRX prescription drug prior form
Navigating the AEBRX prescription drug prior form can bring up many questions. Here are answers to some of the most common concerns:
Additional considerations for patients and healthcare providers
The prior authorization process can significantly impact patient care, often leading to delays in receiving necessary medications. Such delays can affect treatment outcomes and overall patient health. It is vital for healthcare providers to communicate potential wait times to patients, allowing them to manage their expectations effectively.
Patients should be aware of alternative options that may not require prior authorization, particularly for medications that could provide immediate relief. Engaging in discussions with healthcare providers about these alternatives can ensure that patients receive timely care while navigating the complexities of insurance processes.
Recent changes in AEBRX prior forms and policies
The landscape surrounding the AEBRX prescription drug prior form is subject to continuous evolution. Recent updates in regulations and insurance practices directly affect how prior authorization is handled. Insurance companies are increasingly adopting streamlined processes to reduce paperwork and improve patient experiences.
Future trends include a push for more transparency in determination processes, benefiting both patients and healthcare providers. Staying informed on these changes assists stakeholders in navigating the intricate processes associated with prescription drug approvals.
Testimonials and case studies
Understanding the real-world implications of the AEBRX prior authorization process can deepen insight into its intricacies. Healthcare providers and patients alike have shared their experiences, highlighting both challenges and successes.
Success stories often emphasize the ease of using platforms like pdfFiller to manage the AEBRX form, illustrating how technology can streamline documentation workflows and improve patient outcomes. Such testimonials serve as powerful motivators for other healthcare teams to leverage technology in optimizing patient care.
Staying informed
For patient care providers and patients, staying aware of changes to prescription drug policies and paperwork is critical. Providers should engage in ongoing education regarding the prior authorization process and be proactive in updating their practices to address emerging trends.
Resources for continued education include professional healthcare associations, insurance provider updates, and webinars focused on navigating the complexities of prior authorization processes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send aebrx prescription drug prior to be eSigned by others?
How do I edit aebrx prescription drug prior online?
How can I edit aebrx prescription drug prior on a smartphone?
What is aebrx prescription drug prior?
Who is required to file aebrx prescription drug prior?
How to fill out aebrx prescription drug prior?
What is the purpose of aebrx prescription drug prior?
What information must be reported on aebrx prescription drug prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.