Get the free Nc Pharmacy Prior Approval Request for Antiparkinson’s Agents
Get, Create, Make and Sign nc pharmacy prior approval



How to edit nc pharmacy prior approval online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nc pharmacy prior approval

How to fill out nc pharmacy prior approval
Who needs nc pharmacy prior approval?
Understanding the NC Pharmacy Prior Approval Form: A Comprehensive Guide
Understanding the NC Pharmacy Prior Approval Form
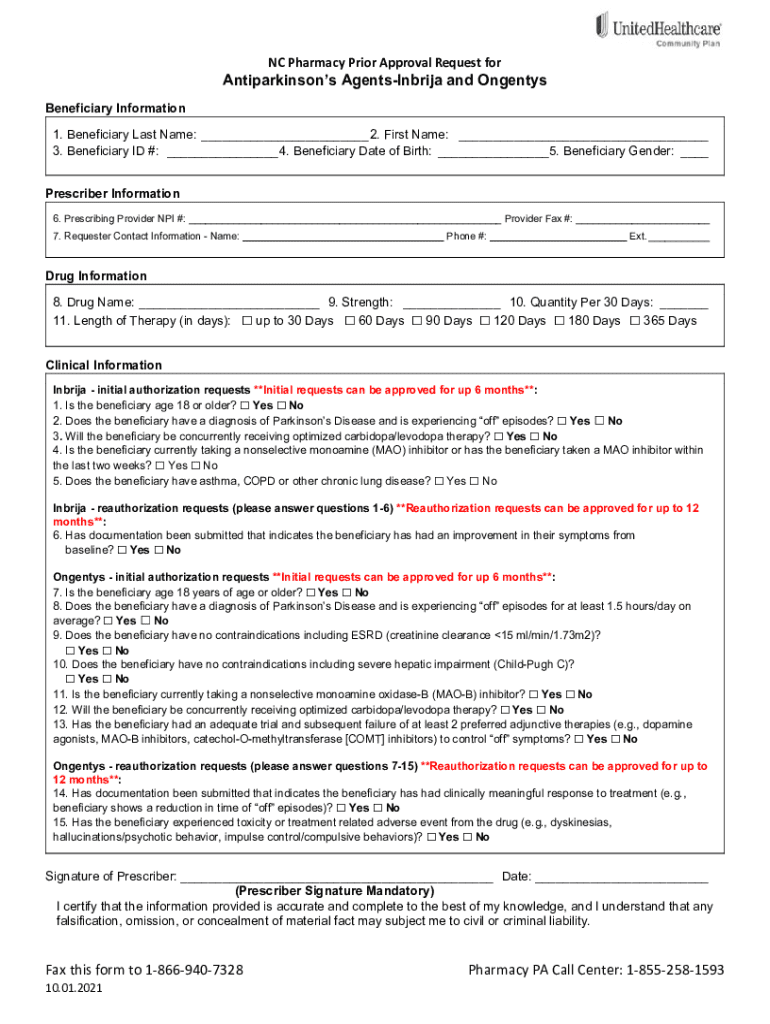
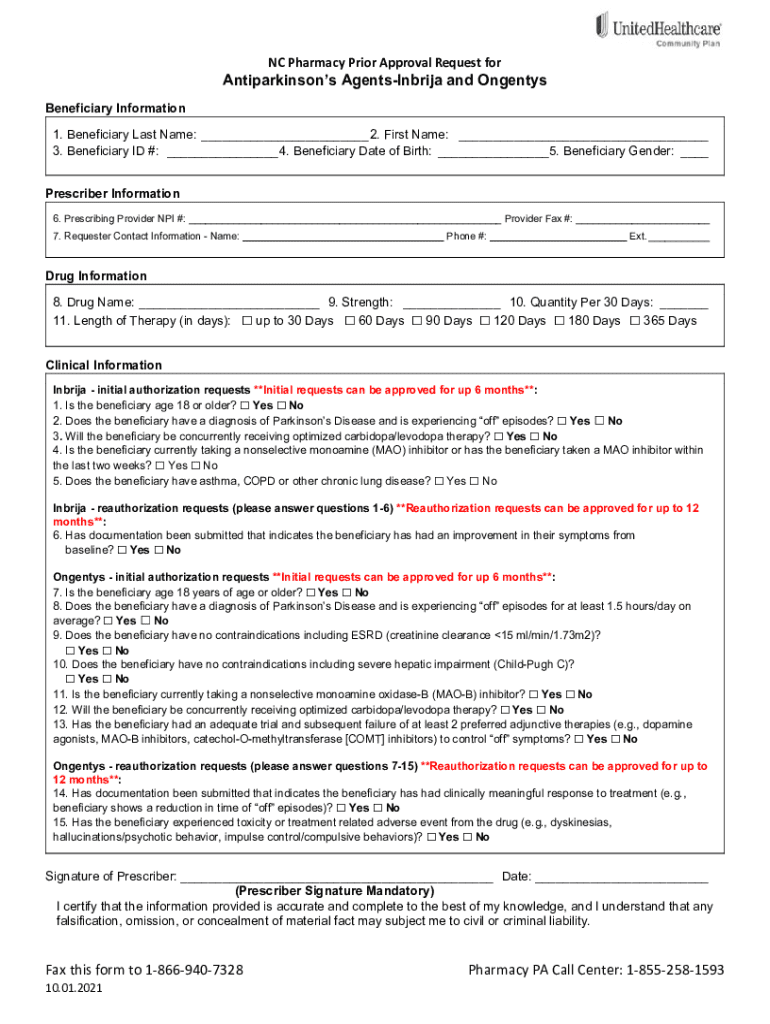
The NC Pharmacy Prior Approval Form serves as a critical tool in facilitating access to essential medications for patients across North Carolina. This document is designed to secure approval from health insurance providers before certain prescriptions can be filled at pharmacies. Its primary purpose is to ensure that the requested medication is medically necessary and aligns with the policy guidelines set forth by the insurance companies.
This form is crucial as it impacts how patients access treatment, ensuring that they receive medications that are both effective and appropriate for their health needs. Additionally, it helps to manage healthcare costs by ensuring that only necessary treatments are approved under insurance plans.
Eligibility criteria
Understanding who qualifies for the NC Pharmacy Prior Approval Form is vital. Typically, this requirement applies to patients needing medications that are high-cost or have alternative therapy options available. Qualifications are usually dictated by the patient's insurance provider's policies, which may vary significantly between plans.
Eligible individuals include those suffering from chronic illnesses, rare diseases, or specific conditions that necessitate the use of certain high-cost medications. Apart from personal medical conditions, eligibility may also hinge on the prescribed drug class and treatment protocols the provider has set.
Common conditions that require prior approval include chronic pain management medications, antidepressants, and certain cancer treatments. It's important to consult with the prescribing physician to ensure that the necessary steps are taken.
Step-by-step guide to completing the form
Completing the NC Pharmacy Prior Approval Form can seem daunting, but it doesn’t have to be. Start by gathering necessary personal and medical information, including your full name, insurance policy number, and detailed medical history relevant to the medication request. This information is crucial as it substantiates the need for the medication in question.
When filling out the form, pay close attention to the instructions provided for each section. Each field is designed to collect specific information that insurance reviewers need. Ensure that you schedule sufficient time to complete the form accurately, as mistakes can lead to delays.
Organizing supporting documentation is equally essential. Common documents include a copy of the prescription, medical records that demonstrate the necessity of the medication, and any relevant lab results. This comprehensive approach to your submission can significantly enhance the likelihood of approval.
Submitting the NC Pharmacy Prior Approval Form
Once the form is completed, the next step is submission. Depending on your insurance provider, you may have multiple options for submitting the form: online through your provider's portal, via mail, or by fax. Be sure to check your insurer's guidelines to determine the best method for your situation.
There are typically deadlines for submission, often aligned with the timelines for medication needs based on treatment regimens. Submitting requests as soon as possible is essential to avoid treatment delays. After submission, the review process engages insurance personnel who will assess your request, often taking anywhere from a few days to a couple of weeks.
Tracking the approval status
Following the submission of the NC Pharmacy Prior Approval Form, it’s important to track the status of your approval request actively. Various methods exist for checking approval status, typically through your insurance provider's online portal or by contacting their customer service directly. Maintaining communication with both your pharmacy and healthcare provider helps ensure the necessary treatment plan continues without interruption.
In instances where there are delays or issues in the approval process, patience is key. However, if you feel that the process is taking too long, it is perfectly acceptable to reach out to your insurance provider for clarification. Having clear, organized records of your submission and communication can help expedite this process.
Understanding the approval decision
Upon review, your request for the NC Pharmacy Prior Approval Form will yield either an approval or denial decision. Understanding these outcomes is crucial. An approval means that your insurance provider has confirmed that the medication is suitable and covered under your plan. You will then receive instructions on proceeding with your pharmacy to fill the prescription.
Conversely, if your request is denied, the denoting information will detail why. Reasons can range from insufficient medical documentation to alternative treatments being available. If you encounter a denial, there is a process for appealing the decision, which typically involves addressing the concerns raised in the denial and resubmitting the request along with any additional necessary documentation.
Resources for assistance
Navigating the NC Pharmacy Prior Approval Form process can be made smoother by leveraging various resources available to you. One of the best starting points is engaging directly with your local pharmacy staff. They can answer specific questions about the submission process and offer insights into common concerns faced by other patients.
Additionally, support can be sought from your healthcare provider, especially if your approval request requires further medical justification or additional documentation. They can often assist in preparing the necessary information to strengthen your case. Online resources, such as your insurance company's website, can provide guidance, answer frequently asked questions, and even offer downloadable forms for convenience.
Common FAQs about the NC Pharmacy Prior Approval Form
The NC Pharmacy Prior Approval Form often leads to several common questions from users. Patients often ask about the duration of the approval process, methods to expedite approvals, or what information is mandatory to include in their request. These FAQs highlight the complexities involved and how communication can make a significant difference.
Providing clear and detailed information can often alleviate uncertainties. Addressing common queries proactively will also assist in avoiding mistakes that lead to delays or denials. Familiarizing oneself with the approval timeline and what each prepares for expectation can assist significantly.
Expert tips for a successful approval process
To maximize your chances of approval with the NC Pharmacy Prior Approval Form, consider utilizing the following expert tips. First, it is wise to attain all supporting documents beforehand and to ensure clarity in your submission to prevent unnecessary complications. The role of your healthcare provider can be instrumental in batch filing the necessary information required for approval.
Additionally, keeping a detailed record of all correspondence and ensuring you have copies of submitted documents. This practice helps in tracing back any questions or issues that arise during the process. Finally, being proactive and promptly following up on your submission can often expedite the review period and lead to faster outcomes.
Conclusion
The NC Pharmacy Prior Approval Form plays a significant role in empowering patients on their health journeys. By understanding the form's requirements and the necessary steps to complete it, individuals can navigate the process of securing medication more efficiently. Utilizing tools like pdfFiller can enhance your experience by simplifying document management, allowing for seamless editing, signing, and collaboration, resulting in a more effective submission that benefits your healthcare journey.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit nc pharmacy prior approval on a smartphone?
How do I edit nc pharmacy prior approval on an iOS device?
How do I complete nc pharmacy prior approval on an iOS device?
What is nc pharmacy prior approval?
Who is required to file nc pharmacy prior approval?
How to fill out nc pharmacy prior approval?
What is the purpose of nc pharmacy prior approval?
What information must be reported on nc pharmacy prior approval?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.