Get the free Medication Prior Authorization Request
Get, Create, Make and Sign medication prior authorization request



How to edit medication prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medication prior authorization request

How to fill out medication prior authorization request
Who needs medication prior authorization request?
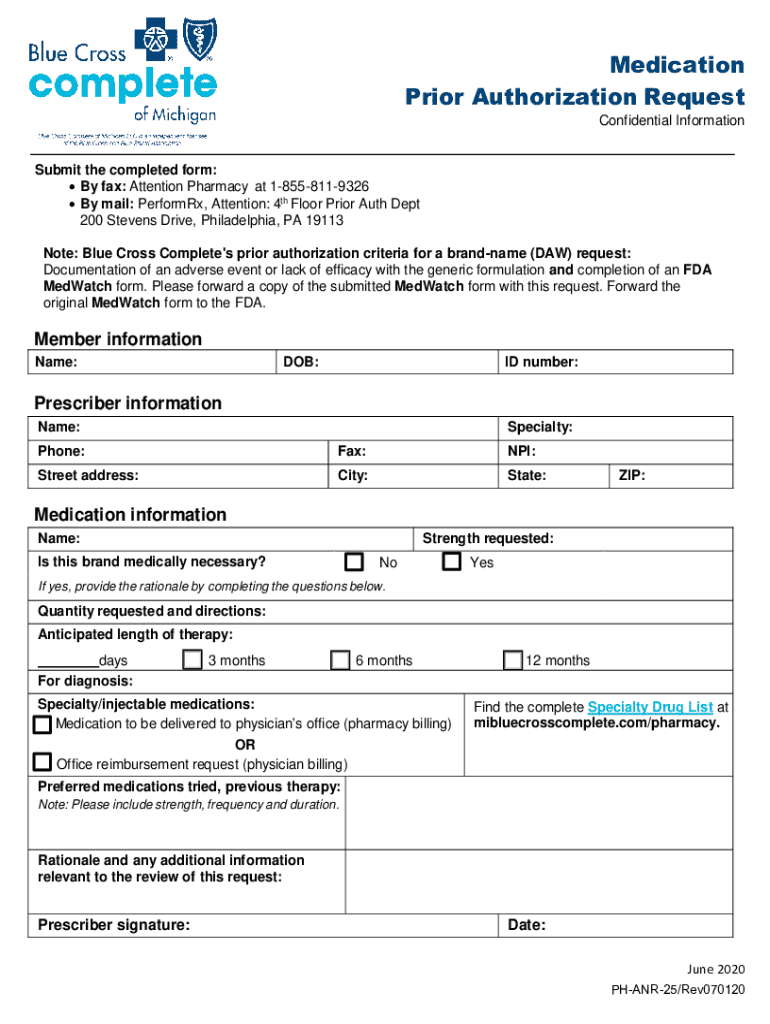
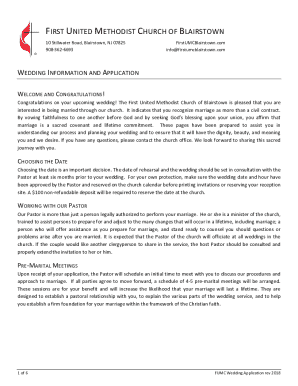
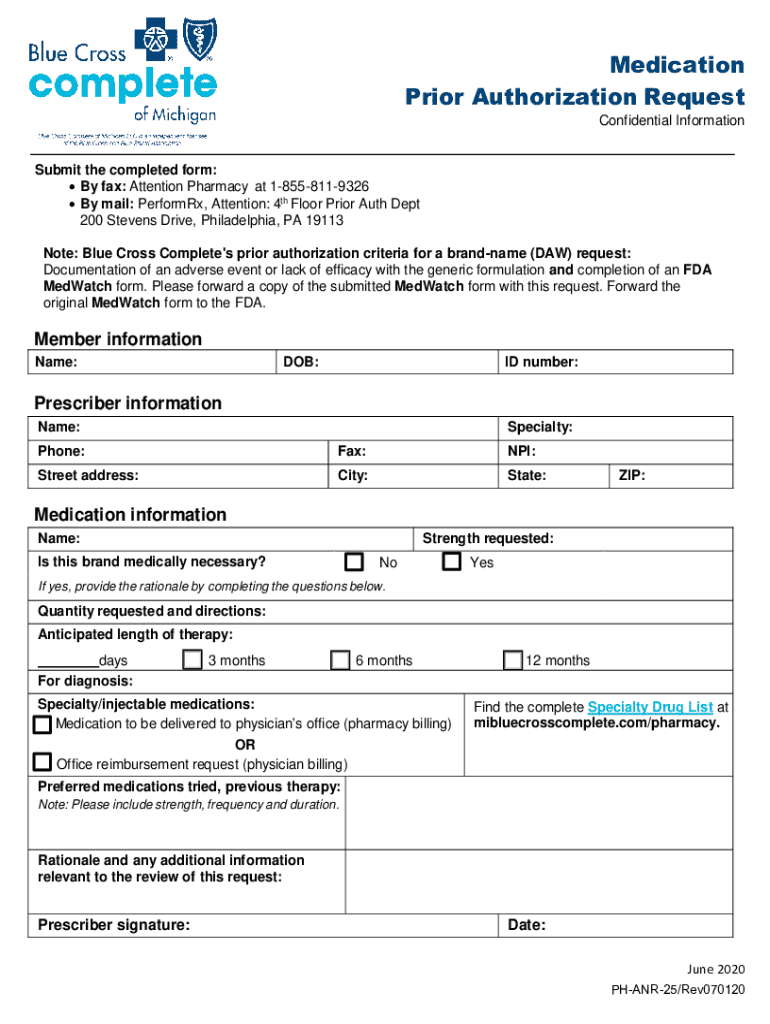
A Comprehensive Guide to the Medication Prior Authorization Request Form
Overview of medication prior authorization
Medication prior authorization (PA) is a process used by insurance companies to determine whether they will cover a prescribed medication. By requiring healthcare providers to submit a prior authorization request form, insurers ensure that prescribed medications meet specific criteria before approving coverage. This procedure serves multiple purposes, primarily patient safety, and cost management within the healthcare system.
The importance of prior authorization lies in its regulation of higher-cost drugs and ensuring that patients receive medications that are medically necessary. It impacts patient care by sometimes delaying the start of necessary treatments, thereby contributing to the complexities of managing a patient's medication regimen while maintaining cost-effectiveness in healthcare delivery.
Key components of a medication prior authorization request form
A medication prior authorization request form typically comprises several essential sections. Each segment requires careful completion to facilitate the approval process and ensure that the insurance provider has all the required information to make an informed decision.
Additionally, specific documentation may be required to accompany the form, such as previous treatment records or lab results, to strengthen the case for authorization.
Step-by-step instructions for completing the medication prior authorization request form
Completing a medication prior authorization request form can be straightforward if approached systematically. Here’s how to do it step-by-step.
Best practices for efficient submission and approval
Navigating the medication prior authorization process can challenge providers and patients alike. To enhance the submission and approval experience, consider the following best practices.
Interactive tools to assist with the process
Technology can significantly streamline the process of managing a medication prior authorization request form. Leveraging tools that simplify documentation handling can improve both efficiency and accuracy.
Collaboration and communication with healthcare providers
Effective communication between patients, providers, and insurers is crucial. Engaging with healthcare providers throughout the process can help ensure a well-rounded approach to submitting prior authorization requests.
Understanding the role of insurance companies
Navigating different insurance policies is essential when dealing with medication prior authorization. Each insurance company has specific protocols that dictate how PAs are handled.
Challenges you may encounter
Encountering obstacles during the prior authorization process is not uncommon. Understanding these challenges helps to formulate effective responses.
Leveraging technology to simplify the process
Integrating technology into the medication prior authorization process can lead to significant improvements in efficiency and error reduction.
Conclusion
Being informed about the medication prior authorization process empowers both patients and providers. Understanding how to correctly fill out the request form is essential for improving the chances of swift approval, which directly affects patient care.
By utilizing pdfFiller’s comprehensive tools, users can significantly simplify the process of creating, managing, and submitting medication prior authorization requests, ultimately fostering better communication and collaboration in healthcare.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my medication prior authorization request in Gmail?
How can I edit medication prior authorization request on a smartphone?
How can I fill out medication prior authorization request on an iOS device?
What is medication prior authorization request?
Who is required to file medication prior authorization request?
How to fill out medication prior authorization request?
What is the purpose of medication prior authorization request?
What information must be reported on medication prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.