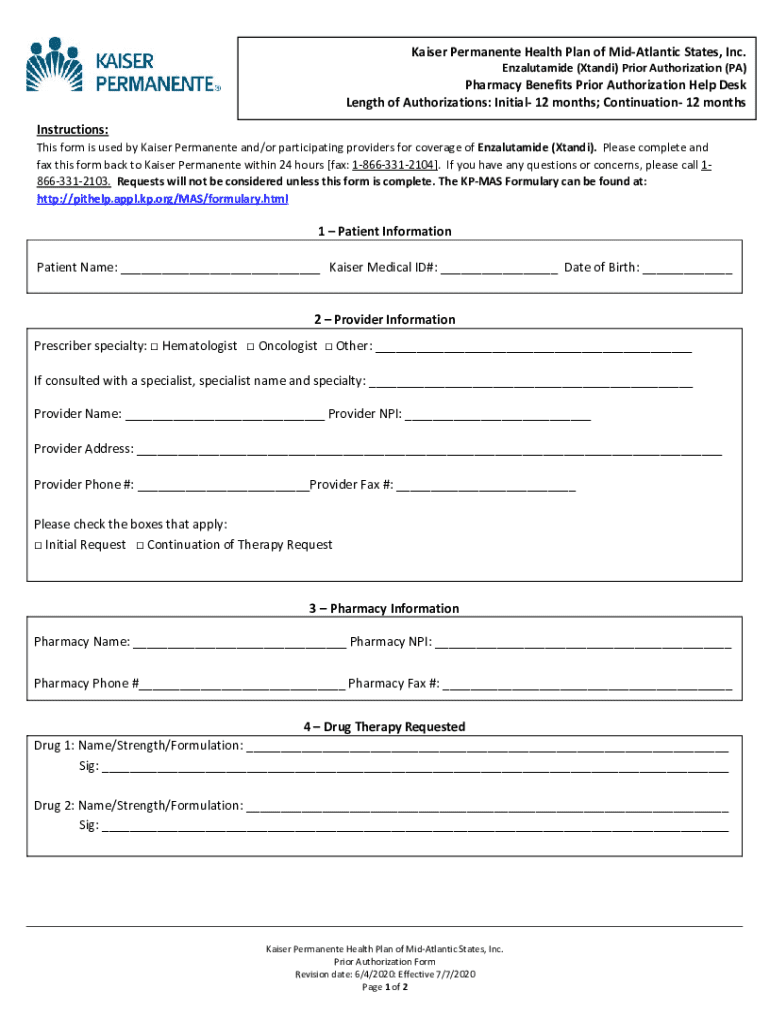
Get the free Kaiser Permanente Prior Authorization
Get, Create, Make and Sign kaiser permanente prior authorization
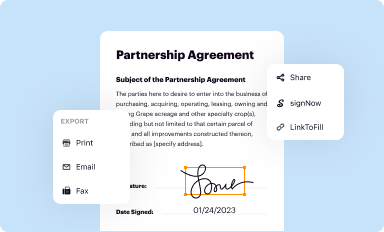
Editing kaiser permanente prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out kaiser permanente prior authorization
How to fill out kaiser permanente prior authorization
Who needs kaiser permanente prior authorization?
Kaiser Permanente Enzalutamide Prior Form: A Comprehensive Guide
Overview of enzalutamide
Enzalutamide is an oral medication prescribed primarily for the treatment of metastatic castration-resistant prostate cancer. It functions by inhibiting several pathways involved in prostate cancer progression, making it a critical component of cancer management for many patients. Understanding the necessity of prior authorization for enzalutamide is vital for both healthcare providers and patients, as it plays a significant role in ensuring that the medication is used effectively while monitoring its appropriateness for each patient's specific circumstances.
Understanding prior authorization
Prior authorization is a process used by healthcare insurers to determine if a prescribed medication is medically necessary before covering it. This step is essential not only for controlling costs but also to ensure that patients receive the most appropriate and effective treatment options. The benefits of a prior authorization system include a structured approach to medication management, reduced waste of healthcare resources, and improved safety for patients by preventing the misuse of powerful medications.
By establishing criteria for approval, prior authorization improves the quality of care as it mandates healthcare providers to provide detailed justification for specific treatments. This process can positively impact patient outcomes by aligning treatment decisions with evidence-based guidelines. However, it can also introduce complexities, such as delays in receiving necessary medications, which require careful navigation to avoid hindering patient care.
Kaiser Permanente's process for enzalutamide
For patients at Kaiser Permanente seeking enzalutamide, understanding the step-by-step process for navigating prior authorization is crucial. This guide outlines how to manage the required approval effectively.
Key information to include in the prior authorization request
To facilitate a smooth prior authorization process for enzalutamide, it is essential to include specific key information in your request. Thoroughly detailing this information can help in obtaining an expedited approval.
Common challenges and solutions in the prior authorization process
While navigating prior authorization is crucial for patient care, it can often present challenges that need to be addressed promptly. Common obstacles include delays in approval, requests for additional information, and potential denials. Addressing these issues requires proactive communication and effective strategies to streamline the process.
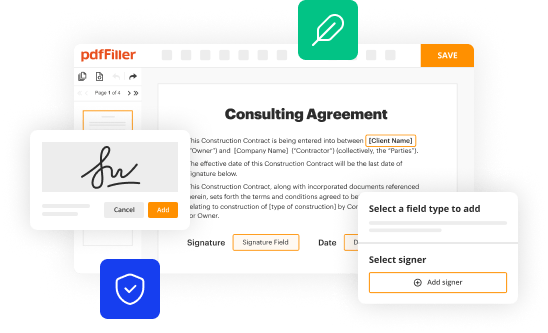
Utilizing pdfFiller for efficient submission
To streamline the process of filling out the Kaiser Permanente enzalutamide prior authorization form, pdfFiller offers a suite of features designed specifically for managing prior authorization requests. Leveraging these tools can make a significant difference in the efficiency and accuracy of submissions.
Interactive tools and resources
Kaiser Permanente provides several resources aimed at aiding the prior authorization process for enzalutamide. Utilizing these resources alongside pdfFiller can enhance your experience significantly.
Case studies: Successful prior authorization for enzalutamide
Reviewing successful prior authorization cases can provide valuable insights. These case studies often highlight strategies that can be replicated in future submissions for enzalutamide.
Frequently asked questions on enzalutamide prior authorization
As with any medical process, questions frequently arise regarding the prior authorization for enzalutamide. Understanding the answers to these common inquiries can alleviate concerns and improve the submission experience.
Conclusion: Empowering users with pdfFiller
The process of obtaining prior authorization for enzalutamide at Kaiser Permanente does not have to be stressful or complicated. By utilizing pdfFiller, users can effectively manage their documents related to enzalutamide and streamline their submissions. The cloud-based platform allows users to easily edit PDFs, collaborate efficiently, eSign documents, and manage everything from a centralized system. This level of organization and accessibility is not only beneficial for healthcare providers but also empowers patients to take an active role in their treatment journey.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit kaiser permanente prior authorization from Google Drive?
How can I edit kaiser permanente prior authorization on a smartphone?
How do I fill out kaiser permanente prior authorization using my mobile device?
What is kaiser permanente prior authorization?
Who is required to file kaiser permanente prior authorization?
How to fill out kaiser permanente prior authorization?
What is the purpose of kaiser permanente prior authorization?
What information must be reported on kaiser permanente prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.