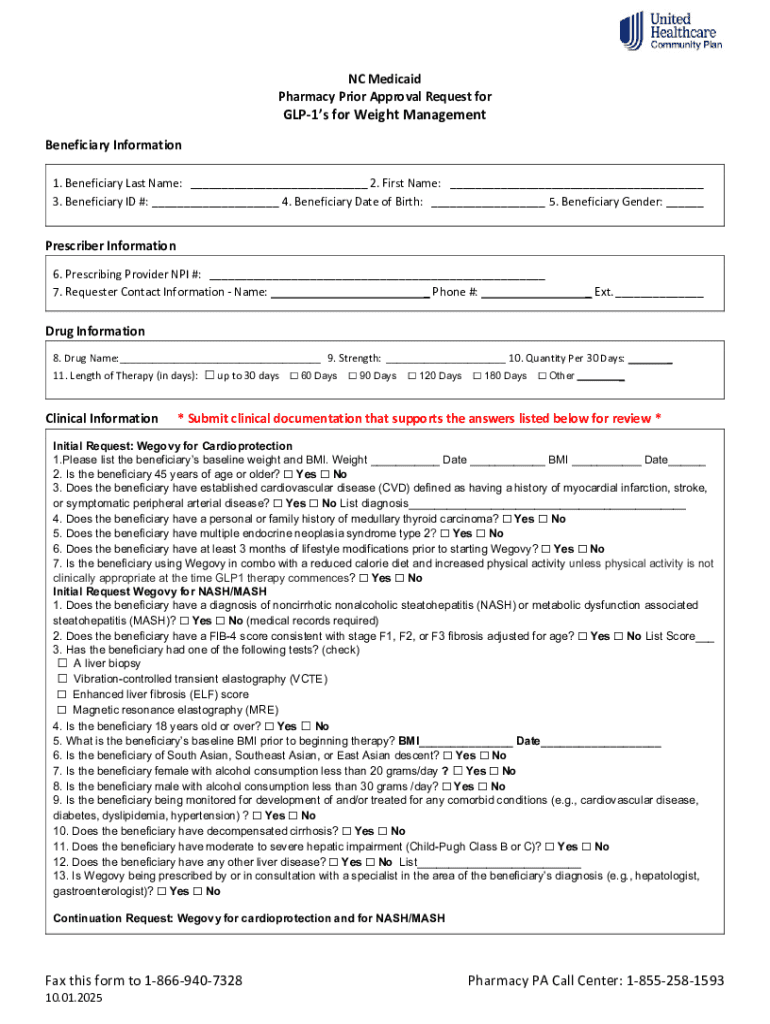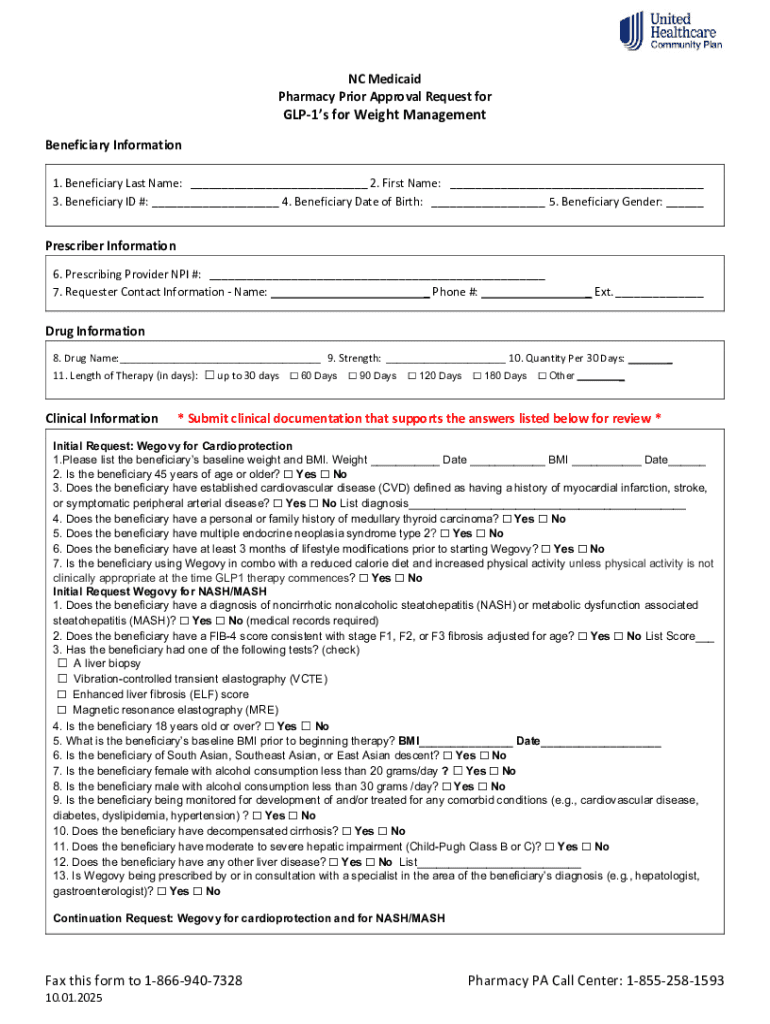
Get the free Nc Medicaid Pharmacy Prior Approval Request for Glp-1’s for Weight Management
Get, Create, Make and Sign nc medicaid pharmacy prior



Editing nc medicaid pharmacy prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nc medicaid pharmacy prior

How to fill out nc medicaid pharmacy prior
Who needs nc medicaid pharmacy prior?
NC Medicaid Pharmacy Prior Form How-to Guide
Overview of the NC Medicaid pharmacy prior authorization process
Pharmacy prior authorization is a critical step in ensuring that NC Medicaid recipients receive the medications they need while also managing costs for the Medicaid program. By requiring prior authorization, the program verifies that certain medications are medically necessary according to established guidelines before they are prescribed.
The importance of this process in NC Medicaid cannot be overstated. It helps prevent prescription drug misuse and ensures that healthcare resources are utilized efficiently. Proper management of medications not only safeguards patient health but also conserves state funding for essential health services.
Key stakeholders in this process include:
Who needs to fill out the prior authorization form?
Any NC Medicaid recipient who is prescribed a medication requiring prior authorization must have this form completed. This includes those who face specific medical conditions or have a history of medication use that necessitates additional scrutiny before the medication is dispensed.
Healthcare providers play a vital role as well; they are responsible for submitting the prior authorization request on behalf of their patients. This collaboration helps ensure that patients receive their medications without unnecessary delays.
Frequently asked questions from recipients and providers often revolve around eligibility criteria, including:
Accessing the NC Medicaid pharmacy prior authorization form
Finding the NC Medicaid pharmacy prior authorization form is essential for both healthcare providers and patients. The form can be easily accessed online through official resources.
Some reliable sources include:
Using pdfFiller for document access has its advantages, including a robust search functionality and mobile access features. This allows users to locate the form easily and fill it out on-the-go, enhancing accessibility.
Step-by-step instructions for completing the pharmacy prior authorization form
Before filling out the NC Medicaid pharmacy prior authorization form, it’s crucial to prepare appropriately. Start by gathering all necessary information, such as patient health records and medication details.
Understanding medical necessity criteria is vital. This helps in justifying the need for the prescribed medication as part of the approval process. Each section of the form must be filled out thoroughly.
Let's explore the detailed walkthrough of the form sections:
Tips for successful submission
Successfully navigating the prior authorization process involves attention to detail. There are common mistakes to avoid when completing the NC Medicaid pharmacy prior authorization form.
Some of these mistakes include:
Best practices for following up on authorization status include maintaining communication with the pharmacy and the prescribing provider. Moreover, utilizing pdfFiller’s features such as eSignature integrations and real-time collaboration tools enhances the submission process, ensuring a seamless experience.
What happens after submission?
Once the NC Medicaid pharmacy prior authorization form has been submitted, the review process commences. Understanding this process is key for recipients and providers alike.
Typically, the review of a prior authorization request takes between 24 to 72 hours. During this time, healthcare professionals assess the provided documentation and justifications for the requested medication.
The outcomes of the review can be categorized into two main types:
Additional considerations and resources
Unmet health-related resource needs in the NC Medicaid program can pose challenges. Many patients do not receive the medications they require due to various barriers, including prior authorization delays.
Training and support for providers is essential in overcoming these challenges. Accessing online webinars and training materials can equip them with the necessary tools and knowledge to navigate the authorization process effectively.
Regional operations and contacts for assistance
For those in North Carolina, knowing where to turn for assistance with the NC Medicaid pharmacy prior authorization process is crucial. Local NC Medicaid offices can provide guidance and support.
Contact information for support includes:






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in nc medicaid pharmacy prior?
How do I complete nc medicaid pharmacy prior on an iOS device?
How do I fill out nc medicaid pharmacy prior on an Android device?
What is nc medicaid pharmacy prior?
Who is required to file nc medicaid pharmacy prior?
How to fill out nc medicaid pharmacy prior?
What is the purpose of nc medicaid pharmacy prior?
What information must be reported on nc medicaid pharmacy prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.