Get the free Nebraska Standard Prior Authorization Request Instructions ...
Get, Create, Make and Sign nebraska standard prior authorization



How to edit nebraska standard prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nebraska standard prior authorization

How to fill out nebraska standard prior authorization
Who needs nebraska standard prior authorization?
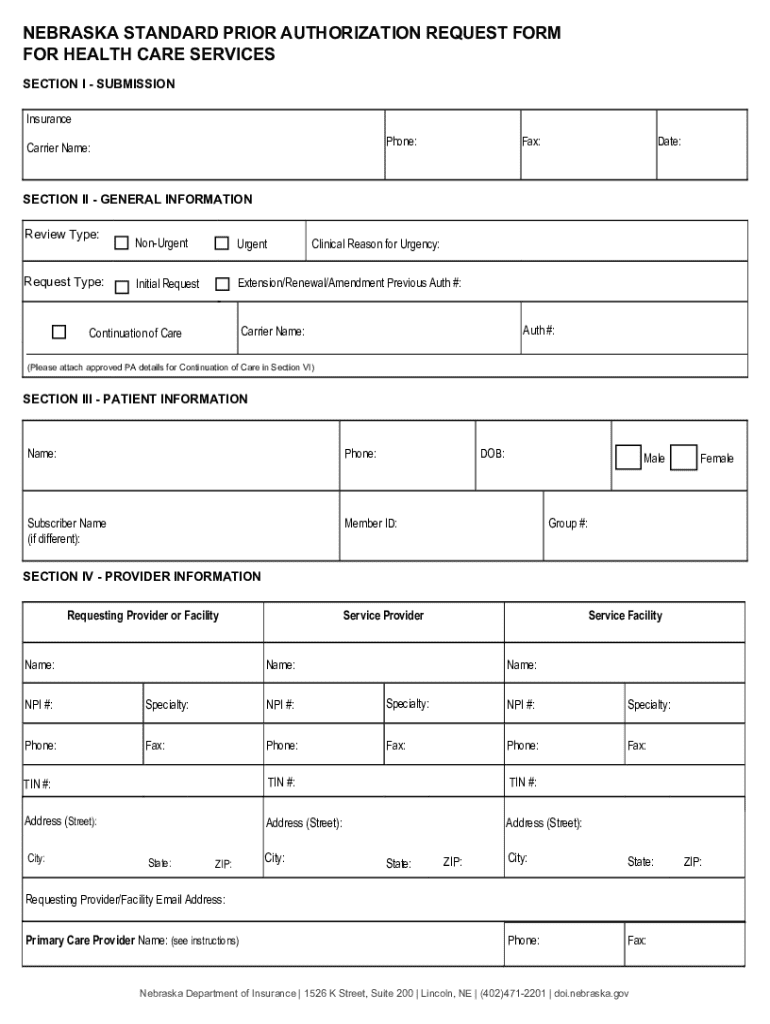
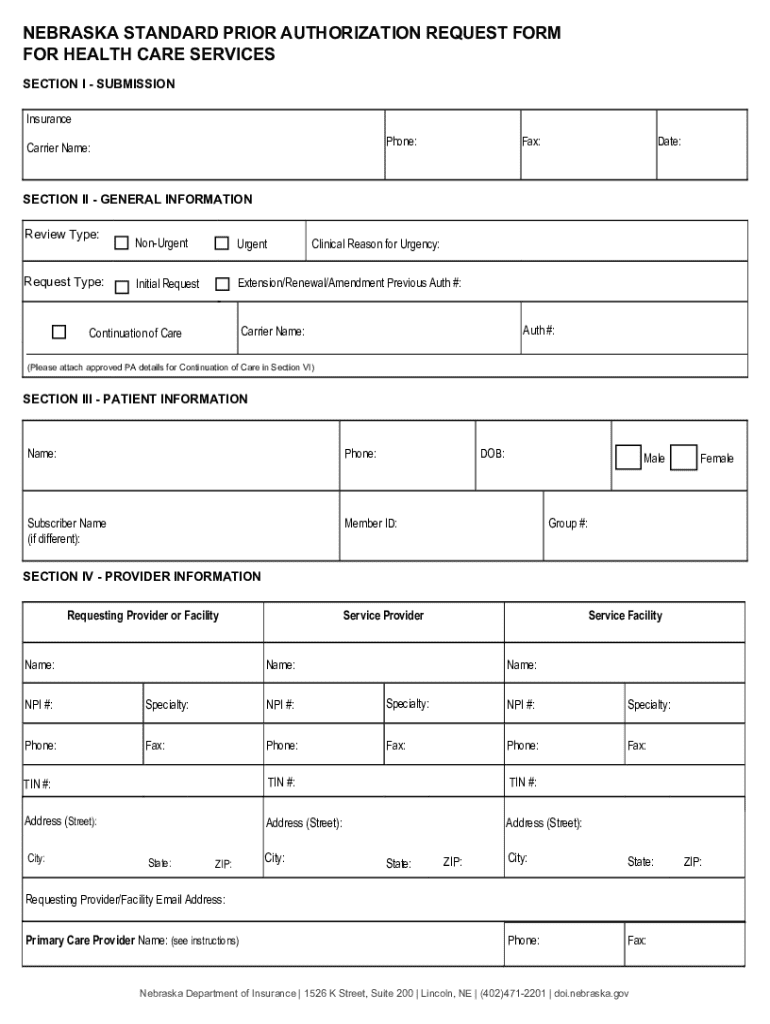
Understanding the Nebraska Standard Prior Authorization Form
Overview of the Nebraska Standard Prior Authorization Form
The Nebraska Standard Prior Authorization Form is an essential document in the healthcare system that facilitates the request for pre-approval of specific medical services or medications. Prior Authorization (PA) serves as a mechanism for insurance companies to manage costs and ensure that patients receive necessary and appropriate care. In Nebraska, this standard form streamlines the process for both healthcare providers and insurance companies, ensuring that medical decisions are guided by clinical necessity.
The significance of using the Nebraska Standard Prior Authorization Form cannot be overstated. It establishes the groundwork for communication between healthcare providers, patients, and insurers, leading to better health outcomes and efficient care delivery. Various services, including advanced imaging, specialist referrals, and certain medications, typically require prior authorization, underscoring the importance of submitting this form accurately.
Who needs the Nebraska Standard Prior Authorization Form?
The Nebraska Standard Prior Authorization Form is essential for various stakeholders within the healthcare system. Primarily, individuals seeking medical services must understand the prior authorization requirements to avoid treatment delays or denials. For patients, this means being informed about the necessity of the form for their care and being proactive in ensuring it is submitted correctly.
Healthcare providers and practitioners play a critical role in the submission of the Nebraska Standard Prior Authorization Form. They must gather necessary patient information, validate medical necessity, and ensure accurate completion of the form to facilitate timely approvals. Lastly, insurance providers and coordinators are involved in reviewing these requests, requiring well-documented submissions to expedite decisions.
Understanding prior authorization
Prior authorization is a cost-control process used by insurance companies to determine whether a specific medical service or medication is covered under a patient's policy. The purpose of this process is to ensure that treatment aligns with the insurance provider’s guidelines and is deemed medically necessary. Patients often find this requirement frustrating, yet it serves a crucial function in managing healthcare costs and maintaining quality of care.
Insurance companies analyze the details provided in the Nebraska Standard Prior Authorization Form to assess the clinical necessity of the requested services. Common reasons for denials include incomplete forms, lack of supporting documentation, or failure to meet established medical criteria. Thus, understanding the requirements of this process from multiple perspectives can greatly improve outcomes.
Key features of the Nebraska Standard Prior Authorization Form
The Nebraska Standard Prior Authorization Form is structured to collect comprehensive information that supports the request for prior authorization. Let's break down its key components:
Additionally, the form requires unique identifiers such as patient ID and authorization numbers to facilitate tracking and processing, making accuracy crucial to avoid delays.
How to fill out the Nebraska Standard Prior Authorization Form
Filling out the Nebraska Standard Prior Authorization Form accurately is critical for approval. Here are step-by-step instructions to ensure a smooth process:
To avoid common mistakes, double-check for missing or misentered information. Common pitfalls include using outdated patient information or neglecting to include necessary clinical justifications.
Submitting the Nebraska Standard Prior Authorization Form
Once the Nebraska Standard Prior Authorization Form is completed, it’s essential to submit it through the appropriate channels. There are typically two methods of submission:
It is essential to be aware of any submission deadlines specific to your insurance provider to prevent delays in treatment and avoid unnecessary stress. Each insurer may have different timelines for reviewing prior authorizations, so familiarize yourself with these details.
Tracking and managing your submission
After submitting the Nebraska Standard Prior Authorization Form, it’s beneficial to track the status of your request. Most insurance companies provide online portals where patients and providers can monitor the progress of their submissions.
Typically, you can expect to receive a decision within a specific timeframe, often ranging from a few days to a couple of weeks. If your request is denied, it's crucial to understand the appeal process, which usually involves submitting additional information or correcting the original request. Resources like pdfFiller can assist in managing appeals efficiently by offering tools that simplify the submission of revised forms.
Using pdfFiller to enhance your experience
Utilizing pdfFiller can significantly simplify the process of completing and managing the Nebraska Standard Prior Authorization Form. This platform offers a range of features that modernize the way patients and providers interact with healthcare documentation.
The cloud-based nature of pdfFiller means that healthcare documentation can be managed from anywhere, making it easier to access and share important information as needed.
Frequently asked questions (FAQs)
Potential questions surrounding the Nebraska Standard Prior Authorization Form often arise as patients and providers navigate the healthcare landscape. Here are some common inquiries:
Tips for a smooth prior authorization process
Navigating the prior authorization process can be challenging, but employing best practices can streamline your experience. Consider the following tips for a successful submission:






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out the nebraska standard prior authorization form on my smartphone?
How do I edit nebraska standard prior authorization on an iOS device?
How do I edit nebraska standard prior authorization on an Android device?
What is nebraska standard prior authorization?
Who is required to file nebraska standard prior authorization?
How to fill out nebraska standard prior authorization?
What is the purpose of nebraska standard prior authorization?
What information must be reported on nebraska standard prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.