
Get the free Nebraska Standard Prior Authorization Instructions for ...
Get, Create, Make and Sign nebraska standard prior authorization
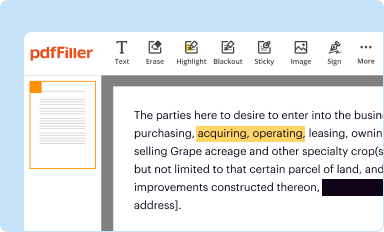
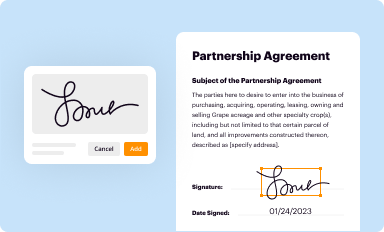
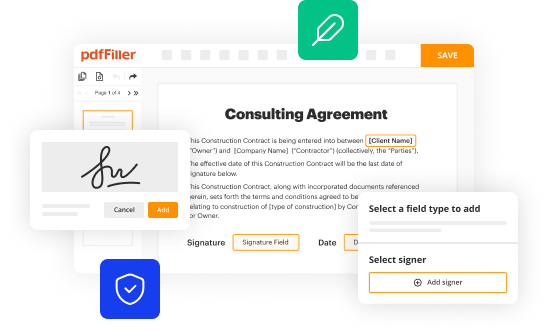
How to edit nebraska standard prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nebraska standard prior authorization
How to fill out nebraska standard prior authorization
Who needs nebraska standard prior authorization?
Nebraska Standard Prior Authorization Form - How-to Guide
Understanding the Nebraska Standard Prior Authorization Form
The Nebraska Standard Prior Authorization Form is a crucial document used in the healthcare realm to ensure that certain medical services or medications are pre-approved before being rendered or dispensed. This form serves as a gatekeeping tool that helps manage healthcare costs and only allows necessary treatments under the insurance protocols.
Understanding the purpose of this form is essential for patients, healthcare providers, and insurers. By requiring prior authorization, insurance companies can assess the medical necessity and appropriateness of a treatment before it incurs costs. This is particularly important in managing specialized and high-cost services such as surgeries, advanced imaging, and new therapies.
The Nebraska Standard Prior Authorization Form is required by insurers, healthcare providers, and patients when requesting coverage for specific services. The aim is to promote appropriate and cost-effective care, thereby minimizing unnecessary expenses for both patients and healthcare systems.
Key components of the Nebraska Standard Prior Authorization Form
The Nebraska Standard Prior Authorization Form contains several key components, each designated to capture vital information necessary for processing requests effectively. Understanding these sections will streamline the completion process and improve the chances of approval.
Completing each section accurately is crucial. It ensures that all necessary information is captured and helps prevent delays or denials during the approval process.
Step-by-step guide to filling out the Nebraska Standard Prior Authorization Form
Filling out the Nebraska Standard Prior Authorization Form can seem daunting, but breaking it down into manageable steps enhances clarity and completion accuracy. Here’s a step-by-step guide to assist you.
Interactive tools and resources for the Nebraska Standard Prior Authorization Form
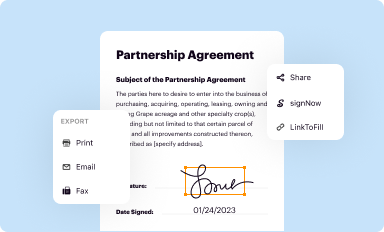
Accessing and managing the Nebraska Standard Prior Authorization Form has been made easier thanks to digital tools and resources available online. pdfFiller offers a wealth of features to assist users in efficiently navigating this necessary paperwork.
Common mistakes to avoid
Filing the Nebraska Standard Prior Authorization Form correctly is paramount, yet many common pitfalls can lead to delays or denials. Being aware of these mistakes can save you valuable time and effort.
Frequently asked questions (FAQs) about the Nebraska Standard Prior Authorization Form
Understanding the Nebraska Standard Prior Authorization Form includes knowing what to expect after submission and addressing common concerns. Here are some frequently asked questions that can guide you.
Best practices for managing prior authorizations
Effectively managing prior authorizations requires organization, follow-up, and perhaps most importantly, an efficient process in place. Below are some best practices to implement.
Enhancing collaboration in prior authorization processes
Collaboration among healthcare providers, insurance representatives, and administrative teams is crucial for efficient prior authorizations. Here are ways to enhance collaboration for better outcomes.
Transitioning to electronic submissions: advantages of using pdfFiller
Transitioning from paper submissions to electronic forms can significantly enhance the prior authorization process. Here are some advantages of using pdfFiller for submitting the Nebraska Standard Prior Authorization Form electronically.
Conclusion: mastering the Nebraska Standard Prior Authorization Form
Mastering the Nebraska Standard Prior Authorization Form is essential for both healthcare providers and patients. With clarity around its purpose, structured guidance on filling it out, and the ease of utilizing pdfFiller, the submission experience can be significantly improved.
By emphasizing accuracy and speed, and leveraging the robust features offered by pdfFiller, users can navigate the complexities of prior authorizations confidently. This ultimately benefits the healthcare system by ensuring patients receive timely and appropriate care without unnecessary delays.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find nebraska standard prior authorization?
How can I fill out nebraska standard prior authorization on an iOS device?
How do I complete nebraska standard prior authorization on an Android device?
What is Nebraska standard prior authorization?
Who is required to file Nebraska standard prior authorization?
How to fill out Nebraska standard prior authorization?
What is the purpose of Nebraska standard prior authorization?
What information must be reported on Nebraska standard prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.















