Get the free Medication Authorization Request Forms (MARF)
Get, Create, Make and Sign medication authorization request forms



Editing medication authorization request forms online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medication authorization request forms

How to fill out medication authorization request forms
Who needs medication authorization request forms?
Medication Authorization Request Forms: A Comprehensive Guide
Understanding medication authorization requests
A medication authorization request refers to a formal request submitted by healthcare providers to insurance companies or payers to obtain approval for certain medications. This process is crucial in ensuring that patients receive appropriate medications that are often subject to specific insurance policies and regulations. It acts as a safety net that balances patient needs with the financial implications for healthcare providers and insurers.
In the healthcare system, medication authorization is vital for several reasons. It helps to manage the costs associated with high-cost therapies and ensures that prescribed treatments align with medical necessity as defined by the insurance plans. However, when authorization requests are not done correctly, it can lead to delays in patient care, increased burden on healthcare providers, and potential adverse effects on patient health.
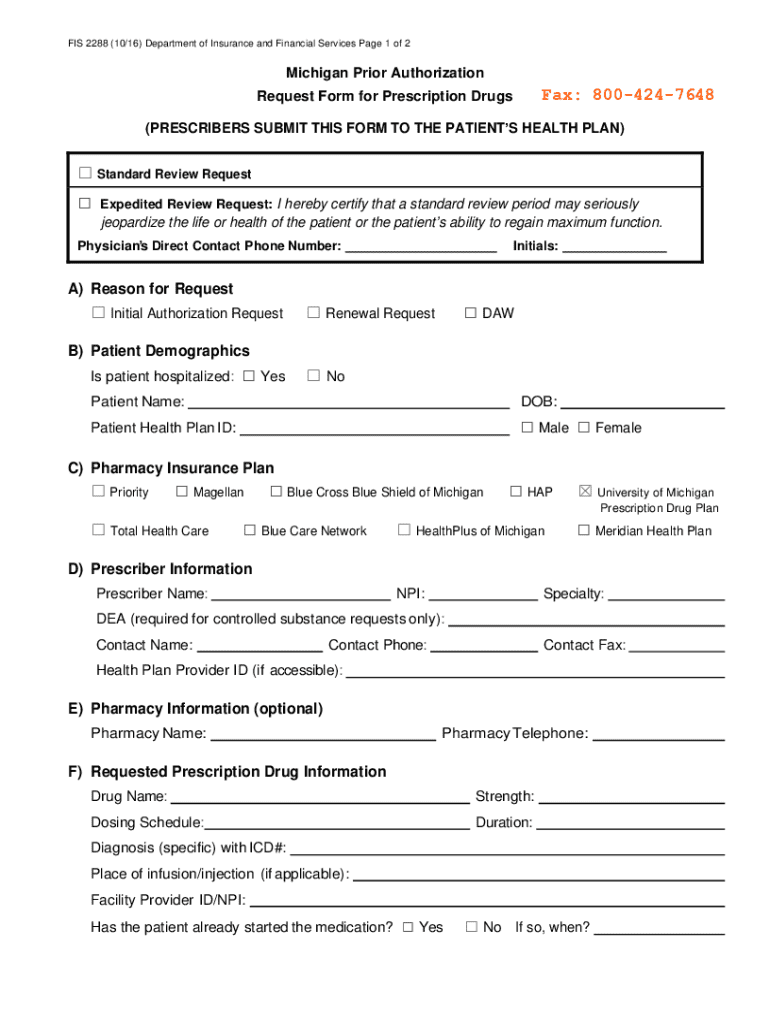
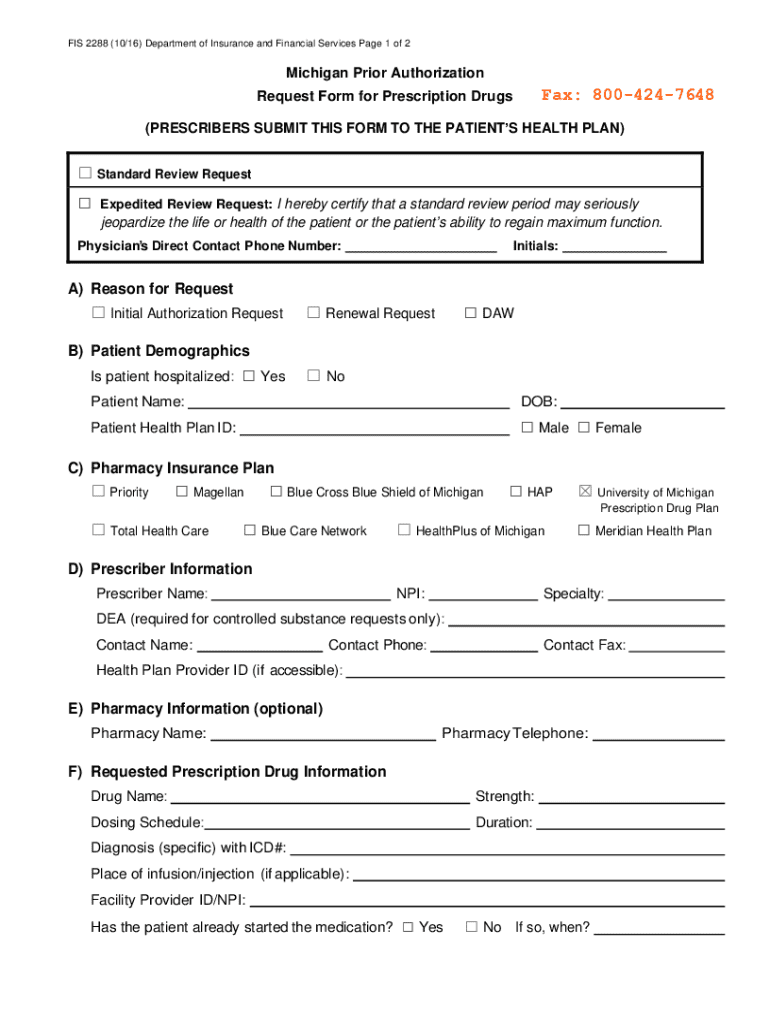
The role of authorization request forms
Authorization request forms serve several crucial functions within the medication authorization process. Primarily, they outline the necessary information that healthcare providers must provide to payers to justify the need for a specific medication. Using standardized forms can streamline communication and improve the efficiency of the approval process.
Several types of medications commonly require authorization requests, particularly those that are high-cost, potentially experimental, or not typically covered under standard healthcare plans. These can include specialty drugs, biologics, and any medications considered off-label for certain conditions. Documentation requirements can vary significantly among payers, leading to common pitfalls where required information is overlooked, causing unnecessary delays.
Step-by-step guide to filling out medication authorization request forms
Pre-submission preparation
Before submitting a medication authorization request, thorough preparation is vital. Collect all necessary documentation, including previous treatment records and relevant test results. This will provide context and support for the requested medication. Confirming patient information such as name, date of birth, and insurance details is crucial to avoid common errors. Additionally, ensure all required signatures from both the prescriber and patient are obtained before submission.
Completing the form
When you begin filling out the authorization request form, ensure that all required sections are completed accurately and comprehensively. Start with the patient details, including their name, date of birth, and insurance information. Next, input the prescriber’s information, including their National Provider Identifier (NPI) and contact details. The medication section should detail the name of the drug, its dosage, and the medical reason for its prescription.
Review and verify
Once the form is completed, conduct a thorough review to double-check all entries. Verify that the request aligns with payer requirements, as it can make or break the authorization outcome. Watch out for common mistakes like missing signatures or incorrect patient information that can lead to unnecessary delays in medication access for patients.
Submitting the authorization request
Submitting a medication authorization request can typically occur through several methods. Many insurers now offer online submission through their provider portals, which is often the preferred method due to its speed and efficiency. Alternatively, requests can also be sent via traditional mail or fax, depending on the payer's requirements. It’s essential to be aware of the submission timelines to ensure timely processing. Following up with the insurer post-submission is a good practice to confirm receipt and clarify any additional information needed.
Different payers have varying preferences regarding submission methods and timelines. Some use specific online platforms to streamline the authorization process, while others still rely on mailed submissions. Familiarizing yourself with these preferences is key to avoiding unexpected delays in the authorization process.
Interpreting authorization outcomes
Approval processes
After submission, providers can expect several outcomes based on the payer's review process. Typical turnaround times for decisions can range from a few days to several weeks, depending on the medication's complexity and the insurer’s workflow. It’s important to have readily accessible resources and contact points in case any additional information or clarification is needed to expedite the authorization process.
Denials and appeals
Not all requests are approved; knowing how to navigate denials is essential. Common reasons for denial can include lack of medical necessity, incomplete forms, or medications not covered under the plan. If a denial occurs, filing an appeal with the proper justification and supporting documentation is the next step. This process usually involves a similar submission process and should be approached systematically for the best results.
Utilizing technology for better management
To optimize the medication authorization request process, leveraging technology can significantly enhance efficiency. Platforms like pdfFiller offer cloud-based document management solutions that allow users to edit, eSign, and manage forms seamlessly. These tools can aid in filling out the authorization request efficiently and tracking the submission process without the complacencies that may come with traditional paperwork.
Interactive tools are available for easy form filling and signing, allowing team collaboration on authorization requests. By integrating technology into workflows, healthcare teams can reduce bottlenecks, minimize errors, and ultimately provide better care to patients requiring authorization for their medications.
Best practices for managing medication authorization requests
To ensure a smooth process, establish best practices for handling medication authorization requests in your organization. Keeping detailed records of each request, including copies of forms and communication with insurers, is crucial. This documentation can serve as a reference point in case follow-ups are needed or issues arise.
Continuing education on policy changes that affect authorization requests helps keep your team up-to-date and compliant with ever-evolving regulations. Establishing clear workflow processes that delineate roles and responsibilities can further enhance efficiency and effectiveness in managing medication authorization requests.
Frequently asked questions about medication authorization requests
Several concerns recur among different individuals regarding medication authorization requests, ranging from the timelines for approvals to the requirements for specific medications. Understanding these common issues may help alleviate the apprehensions healthcare providers face during the authorization process.
Key questions often include inquiries about what to do in case of a prescription denial, how to appeal, and resources for additional guidance. Addressing these concerns with accurate information is essential for building trust and ensuring efficient communication among patients, providers, and insurers.
Case studies: success stories in using authorization forms
Real-world applications of medication authorization request forms often reveal important lessons and insights. There are numerous success stories from clinics and healthcare practices that have optimized their processes, leading to better patient outcomes and increased satisfaction among healthcare providers. Successful cases often highlight the significance of clear communication, thorough documentation, and utilizing technology to improve workflows.
One case study involved a clinic implementing automated systems for tracking authorization requests, yielding a 30% increase in approval rates over six months. Lessons learned from these examples reinforce the importance of ongoing evaluation and proactive adjustments to processes that affect medication authorization workflows.
Enhancing your experience with pdfFiller
pdfFiller stands out as a unique solution for managing medication authorization request forms. With features designed to streamline the process—from form completion and eSigning to comprehensive documentation management—users can navigate authorization requests effortlessly. The platform's user-friendly interface and interactive tutorials empower individuals and teams to maximize their efficiency in handling medication needs.
Testimonials from users indicate that pdfFiller not only improves workflow but also enhances communication with insurers, ultimately leading to faster approvals. Additionally, the platform provides tutorials and interactive demos to facilitate better understanding of the authorization request process, making it an indispensable tool for healthcare providers.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit medication authorization request forms from Google Drive?
How do I make edits in medication authorization request forms without leaving Chrome?
Can I edit medication authorization request forms on an Android device?
What is medication authorization request forms?
Who is required to file medication authorization request forms?
How to fill out medication authorization request forms?
What is the purpose of medication authorization request forms?
What information must be reported on medication authorization request forms?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.