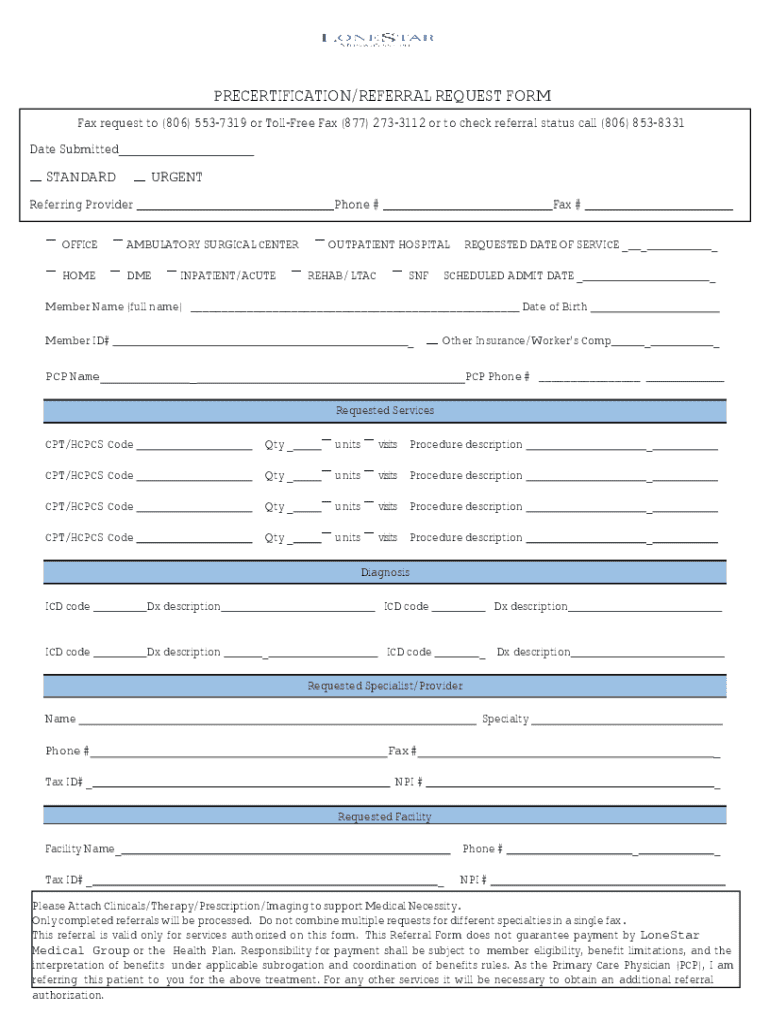
Get the free Pre-Certification Referral Form
Get, Create, Make and Sign pre-certification referral form
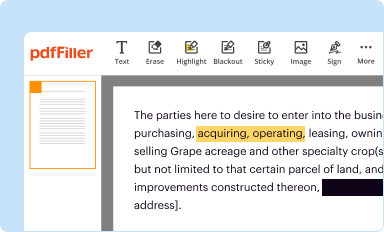
Editing pre-certification referral form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out pre-certification referral form
How to fill out pre-certification referral form
Who needs pre-certification referral form?
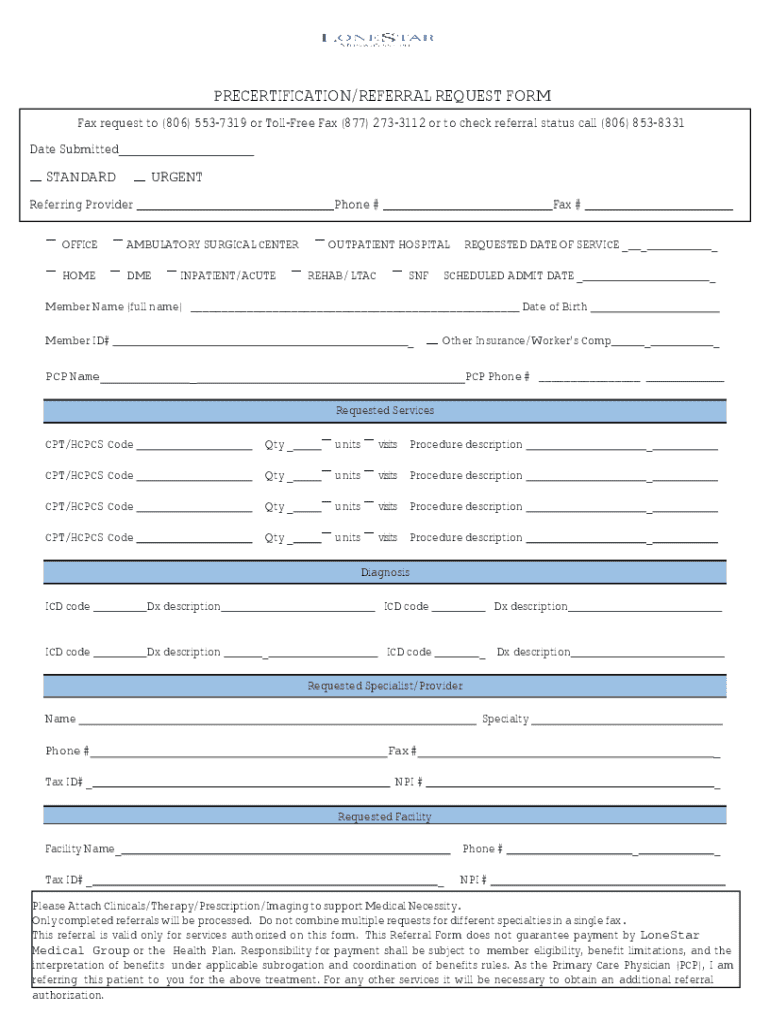
Understanding the Pre-Certification Referral Form for Seamless Healthcare Access
Understanding pre-certification referral forms
A pre-certification referral form is a crucial document in the healthcare system, ensuring that specific medical services are authorized by insurance providers before treatment begins. This form acts as a gatekeeper, streamlining the approval process for necessary medical interventions. Pre-certification is essential because it helps mitigate costs for both the healthcare provider and patient and ensures that the services provided align with the patient's specific insurance coverage.
Common scenarios that necessitate the use of a pre-certification referral form include elective surgeries, advanced imaging techniques like MRIs or CT scans, and specialized treatments such as physical therapy. Some insurance plans require pre-certification even for routine procedures, underscoring its role in managing healthcare costs effectively.
Key components of a pre-certification referral form
When filling out a pre-certification referral form, it's pivotal to include essential information. This begins with patient demographics such as full name, date of birth, insurance provider, policy number, and contact information. Accurate and comprehensive details are vital to ensure smooth processing and avoid delays. Additionally, provider information, including names, National Provider Identifier (NPI) numbers, and contact details, should be meticulously entered.
The treatment information section must specify the procedures or services being requested clearly. This includes the specific codes associated with the requested treatment and a justification explaining why the procedure is medically necessary. This detail is crucial for the insurer's review and helps establish the validity of the request.
Pre-certification requirements
Understanding the varying insurance provider guidelines is crucial when dealing with a pre-certification referral form. Different insurers may have unique requirements regarding what services require pre-approval and the documentation needed. It’s essential to closely review the specific requirements of the patient's insurance company to prevent any processing delays or denial of requests.
Another concept to be aware of is Standardized Episodes of Care (SEOC), which uses specific billing codes to categorize treatments. It plays a significant role in the pre-certification process as certain episodes may demand pre-approval based on their complexity or cost. Medical necessity documentation is equally significant; it should be comprehensive, relevant, and, where possible, supported by clinical evidence or diagnostic test results.
How to request pre-certification
Requesting pre-certification using a referral form involves several systematic steps. First, gather all necessary information and documentation related to the patient's demographics and the proposed treatment. This information serves as the foundation for your application. Completing the pre-certification referral form accurately is the next critical step. Common errors like misreporting patient details or omitting required justification can lead to significant delays.
Following up on your request is just as essential. Regularly checking the status of your pre-certification request keeps you informed about its progress and helps you address any issues that arise promptly. Understanding the typical timeline for pre-certification approvals can alleviate stress and aid in patient scheduling.
Coverage and claims implications
The pre-certification process has direct implications for coverage. Insurers usually outline specific coverage criteria tied to pre-certification approvals. If a service requires pre-certification and is not pre-approved, patients may face out-of-pocket costs that the insurance provider will not cover.
Outcomes of pre-certification requests can vary. An approved request means the service is covered under the terms of the patient’s health plan, allowing the provider to proceed with the treatment. Conversely, denied requests may require an understanding of the reasons behind the denial. Patients have the right to appeal denial decisions, which often involves providing additional information or clarifications to support medical necessity.
Managing your pre-certification documents
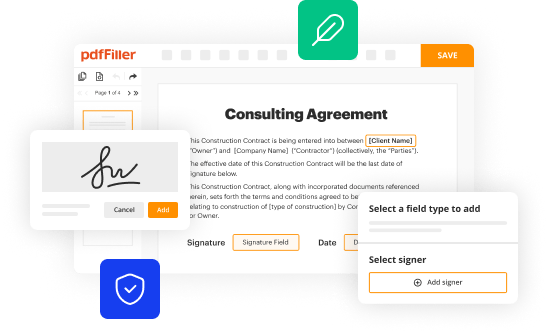
Managing pre-certification documents can be streamlined using pdfFiller's cloud-based platform. This service allows users to edit pre-certification referral forms, collaborate with team members, and securely store documents for easy access. Features that support online editing, e-signatures, and tracking enable seamless workflow and timely submission of forms.
Keeping exhaustive records is essential for future reference. Establish a systematic method for storing pre-certification files to ensure easy retrieval and to support any follow-up inquiries or appeals that may be necessary. Proper documentation management can significantly enhance the efficacy of care transitions and communications between healthcare providers.
Common challenges and solutions
Navigating the pre-certification process isn't without its challenges. Miscommunication with providers or insurers can lead to delays, which could impact patient care timelines. Another common issue is the potential for significant processing delays, resulting from missing information or incorrect submissions.
By adopting these strategies, healthcare providers can effectively reduce the likelihood of issues arising in the pre-certification process, ultimately leading to smoother patient experiences.
Interactive tools and resources
pdfFiller offers various interactive templates specifically designed for pre-certification referral forms. These resources enable users to fill out forms easily, ensuring compliance with specific insurance requirements while saving time in the process. Additionally, integrating online calculators and checklists into the workflow can help estimate approval timelines and set reminders for necessary follow-ups.
Using these tools, healthcare administrators and patient advocates can optimize the pre-certification experience. Easy access to resources helps empower teams to deliver timely care, while templates streamline the often complicated documentation process.
Final considerations
Staying informed about ongoing changes in healthcare policy, particularly regarding pre-certification requirements, is imperative. Insurance companies frequently update their rules, which can significantly impact processing times and requirements. Maintaining an up-to-date understanding equips providers and patients alike to navigate the system more effectively.
Additionally, leveraging community resources such as forums or support groups can offer valuable insights and shared experiences. Engaging with these platforms facilitates knowledge transfer, providing users with useful tools and tips that enhance the pre-certification journey and ultimately lead to improved patient outcomes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send pre-certification referral form to be eSigned by others?
How do I fill out the pre-certification referral form form on my smartphone?
How do I complete pre-certification referral form on an Android device?
What is pre-certification referral form?
Who is required to file pre-certification referral form?
How to fill out pre-certification referral form?
What is the purpose of pre-certification referral form?
What information must be reported on pre-certification referral form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.