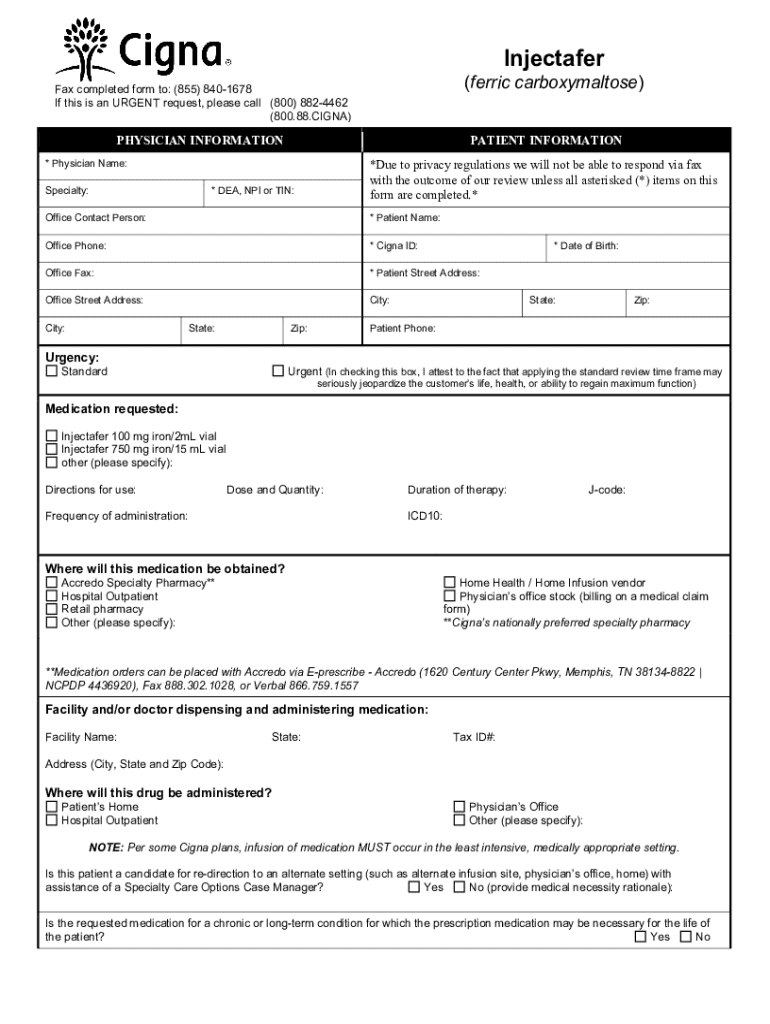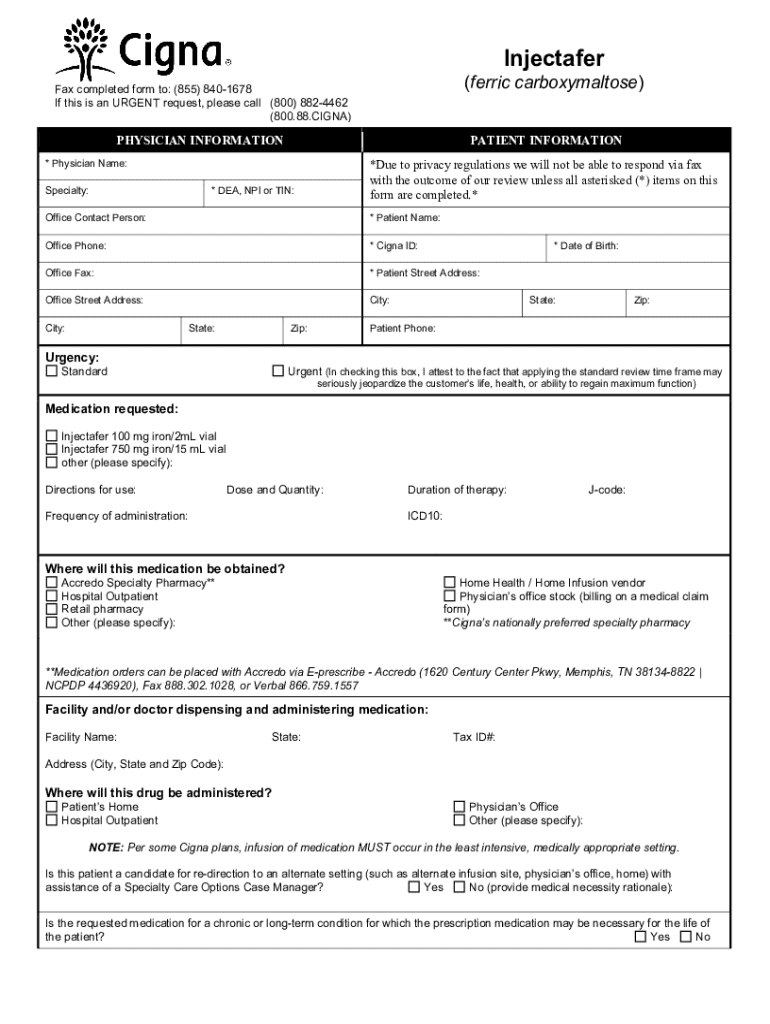
Get the free Injectafer CCRD Prior Authorization Form. Prior Authorization Form for Injectafer
Get, Create, Make and Sign injectafer ccrd prior authorization



Editing injectafer ccrd prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out injectafer ccrd prior authorization

How to fill out injectafer ccrd prior authorization
Who needs injectafer ccrd prior authorization?
Your Guide to the Injectafer CCRD Prior Authorization Form
Understanding prior authorization
Prior authorization is a process used by health insurance companies to determine if they will cover a prescribed treatment or service. This requirement is essential as it allows insurers to assess the medical necessity of the treatment before approving coverage. By implementing prior authorization, healthcare providers are compelled to provide comprehensive justification for the necessity of specific treatments, particularly for high-cost medications like Injectafer—a medication used primarily to treat iron deficiency anemia.
Why Injectafer requires prior authorization
Injectafer (ferric carboxymaltose) is an innovative intravenous iron replacement therapy designed for patients with iron deficiency anemia, especially for those who cannot tolerate oral iron supplements. The requirement for prior authorization when administering Injectafer primarily stems from its high cost and the specificity of its indications. Insurance providers want to ensure that this treatment is only given to patients who meet specific clinical criteria.
Common conditions requiring Injectafer include chronic kidney disease (CKD), inflammatory bowel disease (IBD), and post-surgical recovery in individuals with significant iron deficiency. Each insurance company has its own set of guidelines which outline when prior authorization is essential, often seeing it as a protective measure for both the insurance company and the patient. Moreover, obtaining prior authorization can enhance patient care by ensuring that the prescribed treatment aligns with the latest clinical guidelines.
Navigating the Injectafer CCRD prior authorization process
The prior authorization process for Injectafer can be daunting, but understanding each step can streamline the experience for patients and healthcare providers. Here is a step-by-step guide to obtaining prior authorization:
What information is required on the Injectafer CCRD prior authorization form?
When filling out the Injectafer CCRD prior authorization form, accuracy is key. The form typically includes several mandatory sections, each requiring specific details. Thoroughly completing these sections can significantly affect the approval process.
Providing complete and accurate information is essential for prompt processing. Misfilled forms can lead to delays or denials.
Collaborating with healthcare teams
Collaboration among healthcare providers is crucial in navigating the complexities of the prior authorization process. Clear communication between patients, prescribers, and insurers can minimize delays and enhance treatment outcomes.
Healthcare professionals play significant roles in collecting necessary information and advocating for the patient’s needs during the prior authorization process. Tools like pdfFiller can improve document management, allowing teams to edit, sign, and collaborate on authorization forms efficiently. This platform enables healthcare teams to update documents in real-time, coordinating efforts to expedite the approval process.
Utilizing resources for assistance
Numerous resources are available to assist patients and providers with the prior authorization process. Health insurance companies often provide dedicated helplines for inquiries about coverage and requirements for specific treatments, including Injectafer.
Additionally, online platforms and tools can simplify the management of prior authorization requests. Users can access educational materials, such as guidelines on completing the Injectafer CCRD prior authorization form, to navigate the requirements effectively. Service providers often offer interactive platforms to streamline the management of forms, making it easy to track submission status.
Post-approval steps for Injectafer treatment
Once prior authorization for Injectafer is secured, several critical steps follow. It's essential to coordinate with healthcare providers and schedule a treatment appointment as soon as possible. Making timely arrangements can be vital for patients, particularly those dealing with symptoms of severe iron deficiency.
After treatment, ongoing follow-up care is necessary to monitor the patient’s response to therapy and check iron levels. Regular assessments ensure that the treatment plan remains effective, with adjustments made as necessary based on the patient's feedback and clinical indicators.
Enhancing your document management experience with pdfFiller
pdfFiller offers an array of features designed to simplify the management of prior authorization forms, including the Injectafer CCRD prior authorization form. Users can securely edit, sign, and store important documents all in one cloud-based platform, allowing easy access from anywhere.
Additionally, pdfFiller's collaborative tools enable seamless interactions among team members, ensuring that everyone involved in a patient's care can stay informed and engaged throughout the prior authorization process. Real-time updates and editable PDFs provide an efficient workflow for healthcare teams navigating the complexities of insurance approvals.
Frequently asked questions regarding Injectafer prior authorization
As patients and providers embark on the prior authorization journey, several questions often arise concerning the process, policies, and coverage related to Injectafer. Addressing these inquiries can help demystify the procedure and encourage proactive communication between patients and healthcare professionals.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify injectafer ccrd prior authorization without leaving Google Drive?
How do I make edits in injectafer ccrd prior authorization without leaving Chrome?
How can I fill out injectafer ccrd prior authorization on an iOS device?
What is injectafer ccrd prior authorization?
Who is required to file injectafer ccrd prior authorization?
How to fill out injectafer ccrd prior authorization?
What is the purpose of injectafer ccrd prior authorization?
What information must be reported on injectafer ccrd prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.