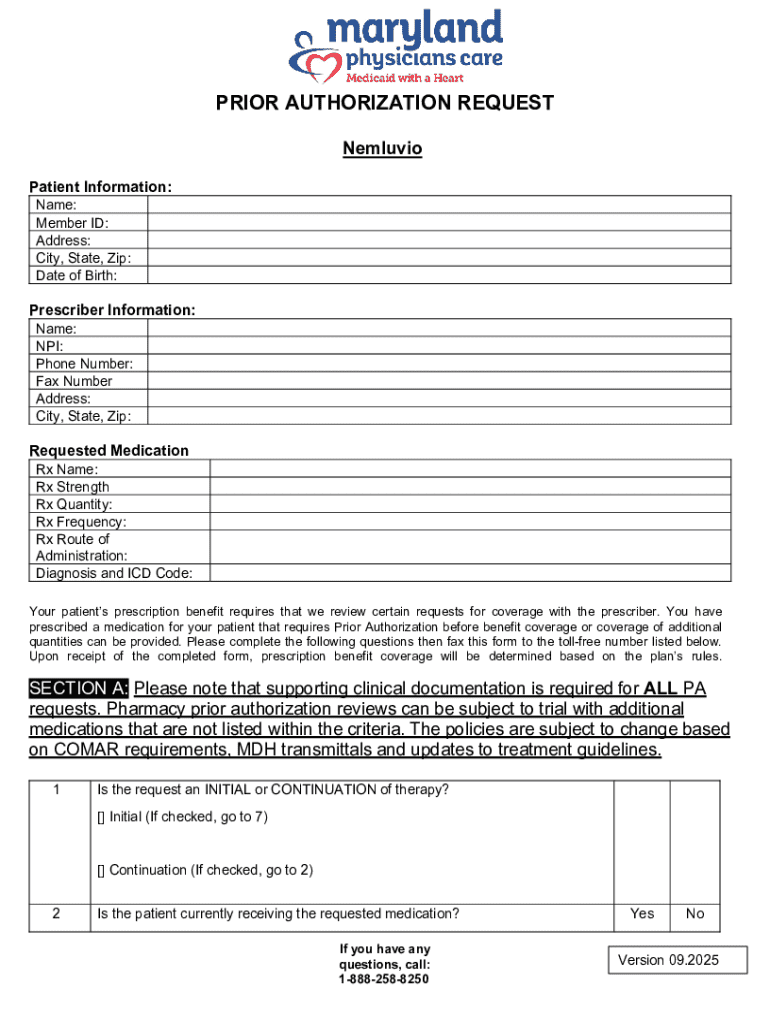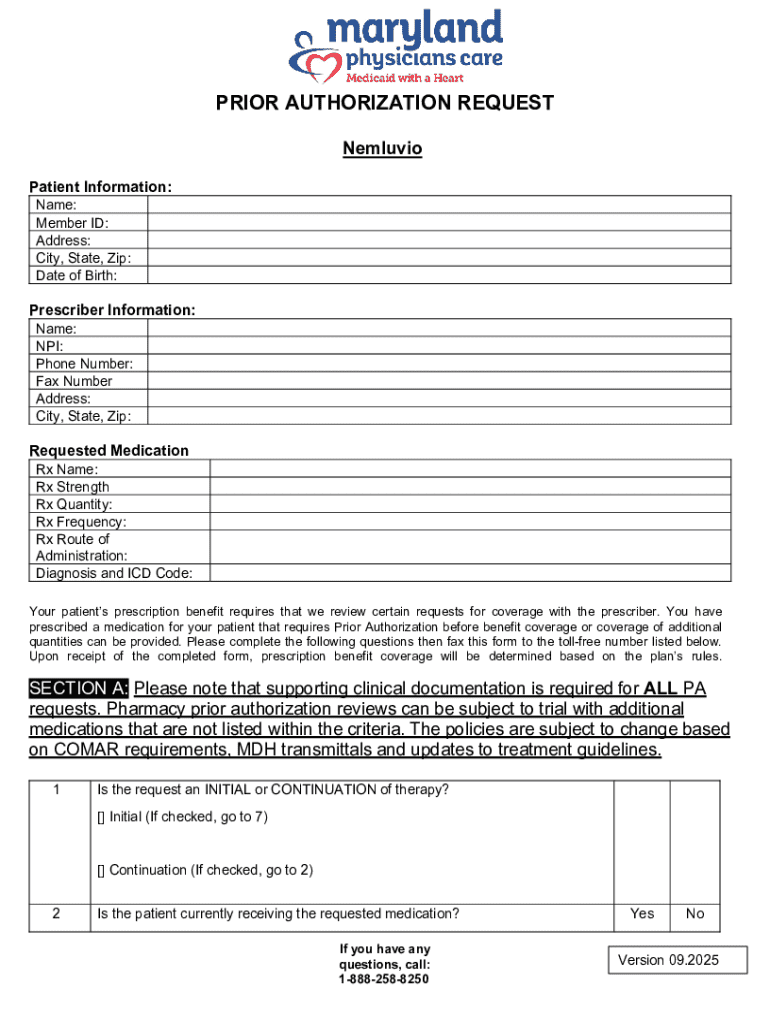
Get the free Nemluvio Prior Authorization Request Form
Get, Create, Make and Sign nemluvio prior authorization request
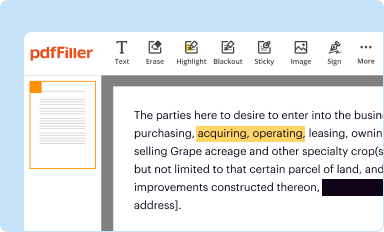
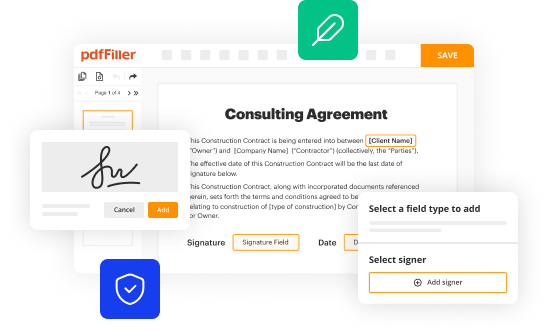
How to edit nemluvio prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nemluvio prior authorization request
How to fill out nemluvio prior authorization request
Who needs nemluvio prior authorization request?
Understanding the Nemluvio Prior Authorization Request Form
Understanding prior authorization
Prior authorization is an essential requirement in the healthcare system, ensuring that specific medical services, prescriptions, or procedures receive the necessary approval from insurance companies before they can be undertaken. This process plays a crucial role in managing costs and ensuring that patients receive appropriate care.
By requiring prior authorization, insurers aim to control healthcare spending and validate the medical necessity of treatments. This not only streamlines costs but also influences how providers prescribe medications and identify treatment protocols. For patients, it can impact timely access to medications, which can be critical for their health.
The Nemluvio prior authorization request form overview
The Nemluvio prior authorization request form is specifically designed for healthcare providers to get approval for Nemluvio, a medication indicated for certain conditions, including Ulcerative Colitis (UC) and Crohn’s Disease. Ensuring the form is filled out correctly is vital, as it significantly increases the chances of approval from insurance providers.
Key components of the Nemluvio form include patient demographics, provider information, medical history related to the condition being treated, and insurance details. Each section serves a specific purpose and must be meticulously filled out to avoid delays or denials.
Detailed instructions for completing the Nemluvio form
Completing the Nemluvio prior authorization request form necessitates careful attention to detail, and this guide provides a step-by-step approach to ensure that all relevant information is accurately captured.
Paying attention to these steps ensures a more streamlined approval process, avoiding common mistakes that can lead to unnecessary delays.
Navigating the submission process
Once the Nemluvio prior authorization request form is completed, submitting it accurately is equally important. Providers should familiarize themselves with the preferred avenues for submission to expedite the review process. Typically, forms can be sent through online portals or via fax.
Following submission, it’s important to establish follow-up procedures. Generally, you can expect feedback within a specific timeframe. Contact the provider’s services for updates to ensure that the process is on track.
Managing denials and appeals
Denials can occur for various reasons, such as incomplete information or the criteria for medical necessity not being met. Understanding the factors that contribute to a denied request can help providers strengthen future submissions.
Being proactive in managing denials not only improves the chances of a successful appeal but also enhances overall efficiency in handling prior authorizations.
Tools and resources for managing forms
Utilizing technology can greatly enhance the management of the Nemluvio prior authorization request form. Platforms like pdfFiller offer interactive tools and resources to facilitate the completion and submission of forms.
These tools not only simplify document management but also enhance collaboration among healthcare teams.
Real-life scenarios and case studies
Examining real-life scenarios helps illuminate the efficacy of the Nemluvio prior authorization process. Many providers have successfully navigated the form's requirements to secure approvals for their patients.
These case studies reinforce the value of thorough preparation and adherence to regulatory guidelines in the prior authorization process.
Frequently asked questions (FAQs)
As with any administrative process, questions often arise regarding the Nemluvio prior authorization request form. Common queries include the specifics of information required, deadlines for submission, and what to do in the event of a denial.
Addressing these questions helps demystify the prior authorization process, ensuring that providers and patients alike are well-informed.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my nemluvio prior authorization request in Gmail?
Can I create an electronic signature for signing my nemluvio prior authorization request in Gmail?
Can I edit nemluvio prior authorization request on an iOS device?
What is nemluvio prior authorization request?
Who is required to file nemluvio prior authorization request?
How to fill out nemluvio prior authorization request?
What is the purpose of nemluvio prior authorization request?
What information must be reported on nemluvio prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.